Cytokine and Lymphokine Studies
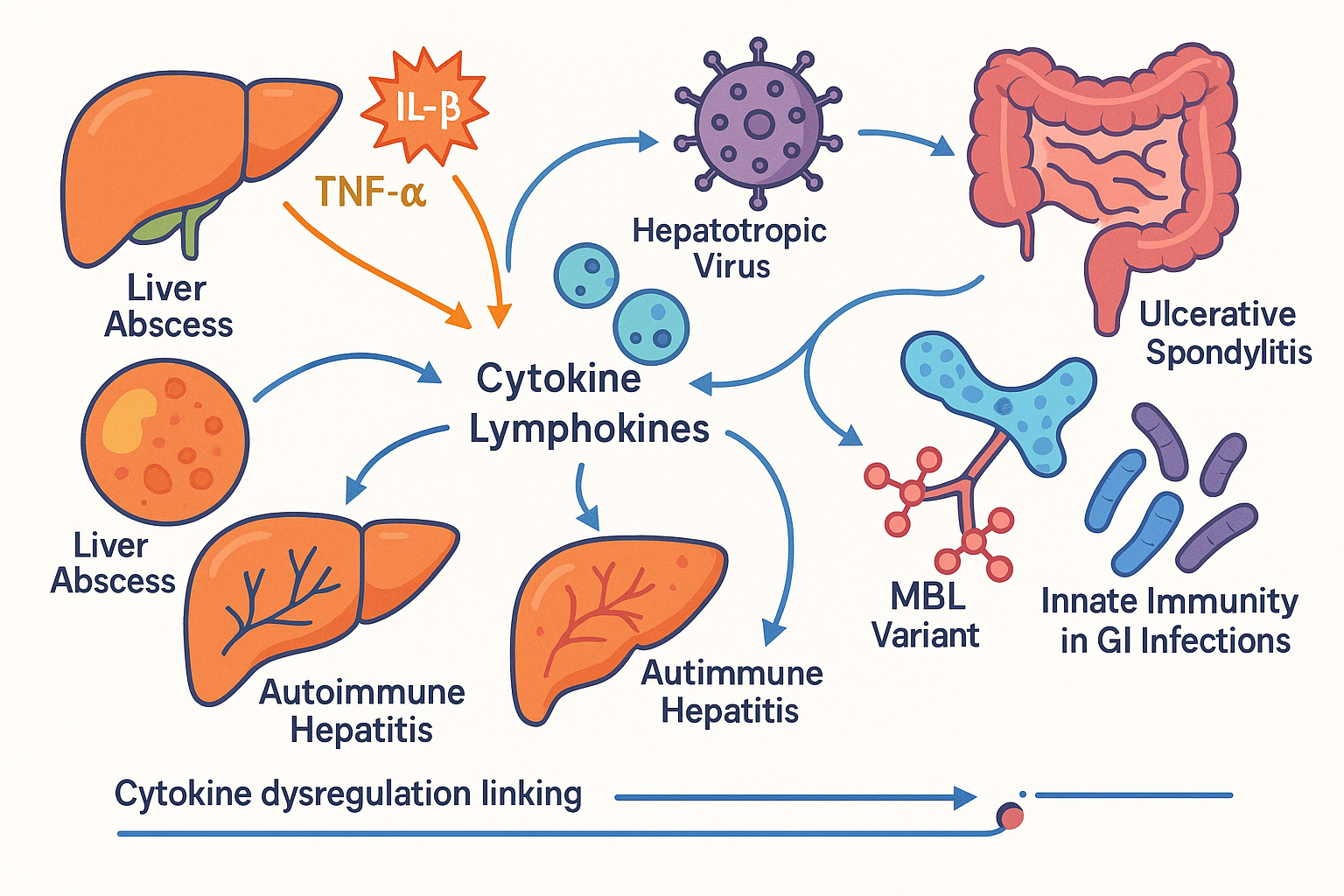
The Centre for Liver and Related Diseases (CLRD) has cultivated deep expertise in immunopathology with a focus on cytokines and lymphokines that orchestrate inflammation, immune signaling, and tissue repair across hepatic and gastrointestinal conditions. Central mediators such as interleukin‑1 beta (IL‑1β), tumor necrosis factor‑alpha (TNF‑α), and lymphokines from Th1, Th2, and Th17 lineages define disease trajectories in liver abscess, viral and autoimmune hepatitis, and systemic inflammatory states including sepsis, ulcerative colitis, and ankylosing spondylitis. Over years of translational research, CLRD has systematically mapped cytokine networks, correlated immune signatures with clinical phenotypes, and integrated genetic insights most notably through the analysis of mannose‑binding lectin (MBL) variants to understand the innate immune determinants of gastrointestinal infections. This body of work underpins CLRD’s capability to move from bench to bedside: identifying actionable biomarkers, refining prognostic algorithms, and shaping personalized, immune‑guided treatment pathways that improve outcomes.
Liver Abscess: Immunologic Profiling and Guided Intervention
Liver abscess represents a high‑risk, localized infectious process, bacterial or amoebic, marked by robust neutrophilic infiltration, tissue necrosis, and the potential for systemic spread. CLRD’s cytokine mapping in abscess disease consistently shows heightened IL‑1β and TNF‑α activity, a pattern that mirrors clinical severity and correlates with purulent burden, fever, and hemodynamic instability. By coupling immune profiling with precision diagnostics, CLRD employs contrast‑enhanced ultrasonography and cross‑sectional imaging to define cavity architecture, and uses image‑guided aspiration or catheter drainage to achieve source control when indicated. Antimicrobial therapy is tailored to etiology covering enteric Gram‑negative flora and anaerobes in pyogenic cases or metronidazole‑based regimens in amoebic disease, while immunologic insights inform adjunctive strategies to temper excessive inflammation. In patients demonstrating high cytokine activity with evolving systemic signs, CLRD clinicians institute close hemodynamic monitoring, optimize fluid resuscitation, and reconcile host immune status with pathogen dynamics, thereby reducing complications such as rupture, peritonitis, and sepsis. This integrated approach, microbiologic stewardship, procedural expertise, and cytokine‑aware care, has enabled earlier resolution and fewer relapses.
Viral Hepatitis: Immune Signatures and Personalized Antiviral Care
Hepatitis B and C infections provoke immune responses that determine whether viral clearance is achieved or chronicity ensues. CLRD’s research demonstrates that the immune landscape in acute hepatitis is dominated by brisk pro‑inflammatory cytokine activity, whereas chronic phases reveal persistent, dysregulated lymphokine signaling that sustains low‑grade inflammation, fibrogenesis, and immune exhaustion. Translating these insights into clinical practice, CLRD combines guideline‑concordant antiviral therapy, direct‑acting antivirals for HCV and nucleos(t)ide analogs for HBV, with immune profiling to identify patients at risk of aggressive necroinflammation or accelerated fibrosis. Where cytokine overactivity is driving hepatocellular injury, care plans emphasize close monitoring of transaminases, judicious steroid use in select immune‑mediated flares, hepatoprotective strategies, and lifestyle modifications to reduce co‑factors such as alcohol and metabolic stress. For patients with virologic suppression but ongoing inflammatory signatures, CLRD explores adjunctive immunomodulation, anticipates extrahepatic manifestations, and coordinates long‑term surveillance to preempt progression to cirrhosis or hepatocellular carcinoma. The center’s synthesis of virology, immunology, and longitudinal care has produced durable virologic responses with measurable improvement in inflammation and fibrosis staging.
Autoimmune Hepatitis: Targeted Immunomodulation and Durable Remission
Autoimmune hepatitis is distinguished by lymphocyte‑mediated hepatocellular injury and autoantibody formation, frequently driven by Th1 and Th17 lymphokines that sustain chronic portal and lobular inflammation. CLRD’s work profiles these immune axes to clarify disease activity, relapse risk, and response to therapy. Treatment begins with induction using corticosteroids to quickly quell inflammation, followed by steroid‑sparing immunosuppressants such as azathioprine to achieve biochemical remission and histologic healing. In patients with refractory disease or steroid intolerance, CLRD deploys second‑line agents mycophenolate mofetil, tacrolimus or considers biologics that selectively inhibit cytokine signaling where appropriate. Cytokine‑guided monitoring informs taper schedules and relapse surveillance, while patient‑centric measures address bone health, infection risk, and metabolic side effects. By integrating immune signatures into routine management, CLRD has improved remission durability, reduced flare frequency, and optimized quality of life with fewer cumulative steroid doses.
Sepsis and Systemic Inflammation: Early Recognition and Cytokine‑Aware Support
Sepsis represents a dysregulated, life‑threatening host response characterized by surges in IL‑1β, TNF‑α, and other mediators that precipitate endothelial disruption, coagulopathy, and multi‑organ dysfunction. CLRD’s focus on cytokine dynamics equips clinicians to recognize early systemic escalation in patients with liver disease, where baseline immune perturbations increase vulnerability. Management is anchored in rapid source control, timely broad‑spectrum antibiotics tailored by local ecology and de‑escalated with microbiologic data, and structured organ support in accordance with critical care best practices. In select scenarios and clinical trials, cytokine‑modulating strategies are considered to dampen hyperinflammation, always balanced against infection clearance. The center’s standardized sepsis bundles, hemodynamic optimization, and vigilant immune‑status tracking have reduced ICU transfers and improved survival in vulnerable hepatic cohorts.
Ulcerative Colitis and Ankylosing Spondylitis: The Gut–Joint Axis and Biologic Precision
Ulcerative colitis and ankylosing spondylitis share convergent inflammatory circuits involving TNF‑α and IL‑17, demonstrating how mucosal immunity can intersect with axial skeletal inflammation. CLRD utilizes this understanding to coordinate care across gastroenterology and rheumatology, deploying biologic therapies that neutralize these cytokines and thereby achieve mucosal healing, reduce joint inflammation, and prevent structural damage. For ulcerative colitis, induction and maintenance regimens are selected based on disease extent, severity, and biomarker profiles, while fecal calprotectin and endoscopic assessment track healing. In ankylosing spondylitis, imaging of sacroiliac joints and spinal involvement pair with inflammatory markers to guide therapy onset and escalation. Nutritional counseling, microbiome‑supportive strategies, and exercise therapy complement biologics to maintain remission and functional mobility. CLRD’s immune‑aligned protocols have resulted in better symptom control, fewer hospitalizations, and sustained patient‑reported outcomes across gut and joint domains.
Innate Immunity in GI Infections: MBL Variants and Susceptibility‑Driven Care
Mannose‑binding lectin is a pivotal pattern‑recognition molecule in the lectin complement pathway, and genetic polymorphisms can influence protein levels, opsonization efficacy, and infection susceptibility. CLRD’s variant analysis correlates MBL genotypes and phenotypes with clinical courses of gastrointestinal infections, demonstrating how innate immune differences affect pathogen clearance and reinfection risk. These insights inform preventive and therapeutic strategies: vaccination schedules are prioritized where available, antimicrobial choices are made with consideration of host defenses, and prophylaxis or early intervention is planned for high‑risk individuals. When recurrent infections coincide with low MBL activity, clinicians strengthen barrier protection, optimize nutrition and micronutrient status, and monitor for complications such as post‑infectious irritable bowel syndrome or inflammatory sequelae. The result is a model of care that pairs genetics with clinical vigilance to reduce morbidity.
CLRD’s Capabilities and Methods of Treatment
CLRD’s capabilities arise from the integration of advanced diagnostics, immune analytics, interventional expertise, and comprehensive clinical pathways. At the diagnostic level, the center offers high‑resolution ultrasonography, contrast‑enhanced CT and MRI for hepatobiliary evaluation, and image‑guided procedures for abscess drainage and tissue sampling. Laboratory capability includes cytokine panels covering IL‑1β, TNF‑α, IL‑6, IL‑17, interferons, and chemokines; flow cytometry for lymphocyte subset analysis; and molecular assays for viral load quantification and autoantibody profiling. Genetic testing platforms assess MBL polymorphisms and other innate immunity markers to anticipate infection risk and personalize care. Therapeutically, CLRD delivers precision antimicrobial regimens aligned with culture data and local resistance patterns, antiviral therapy tailored to genotype and fibrosis stage, structured immunosuppression for autoimmune hepatitis, and biologic agents that target TNF‑α or IL‑17 pathways in inflammatory bowel and spondyloarthropathies. Procedural capabilities include ultrasound‑ or CT‑guided aspiration and catheter drainage for liver abscesses, portal pressure assessment when indicated, and endoscopic evaluation for colitis activity. Supportive care spans nutrition optimization, hepatoprotective strategies, vaccination planning, and coordinated rehabilitation for musculoskeletal recovery. Care models are multidisciplinary and protocol‑driven, blending evidence‑based medicine with individualized immune insights to minimize flares, prevent complications, and improve long‑term outcomes. Continuous quality measurement and prospective registries ensure that therapeutic decisions are audited for effectiveness and safety, allowing CLRD to iterate and refine practice standards.
CLRD’s specialization in cytokine and lymphokine studies places the center at the forefront of immunologically informed care for liver and related diseases. By connecting detailed immune profiling with advanced diagnostics and targeted therapies, CLRD has established a translational pipeline that moves discoveries from research publications into daily clinical practice. Patients benefit from earlier diagnosis, more precise risk stratification, and treatments aligned with their immune signatures, while the health system benefits from reduced complications, fewer hospitalizations, and improved functional outcomes. As CLRD continues to expand its registries, refine cytokine‑guided protocols, and integrate genetic insights such as MBL variant analysis, the center will deepen its impact across hepatic and gastrointestinal medicine. This preface frames the capability and scope of CLRD’s work; subsequent individual pages for each disease will present specific pathways, evidence summaries, and patient‑centric protocols derived from the center’s research portfolio and clinical experience.
