Circulating Immune Complexes
Circulating Immune Complexes (CICs) represent antigen-antibody aggregates that remain in systemic circulation when clearance mechanisms such as the reticuloendothelial system are overwhelmed or impaired. Their persistence leads to deposition in target tissues, triggering complement activation and inflammatory cascades. In autoimmune liver diseases, CICs contribute to hepatocellular injury and fibrosis, while in peptic ulcer disease, they exacerbate mucosal immune dysregulation and chronicity. The clinical significance of monitoring CICs lies in their ability to reflect ongoing immune activity, predict disease progression, and guide therapeutic interventions.
What Are Circulating Immune Complexes?
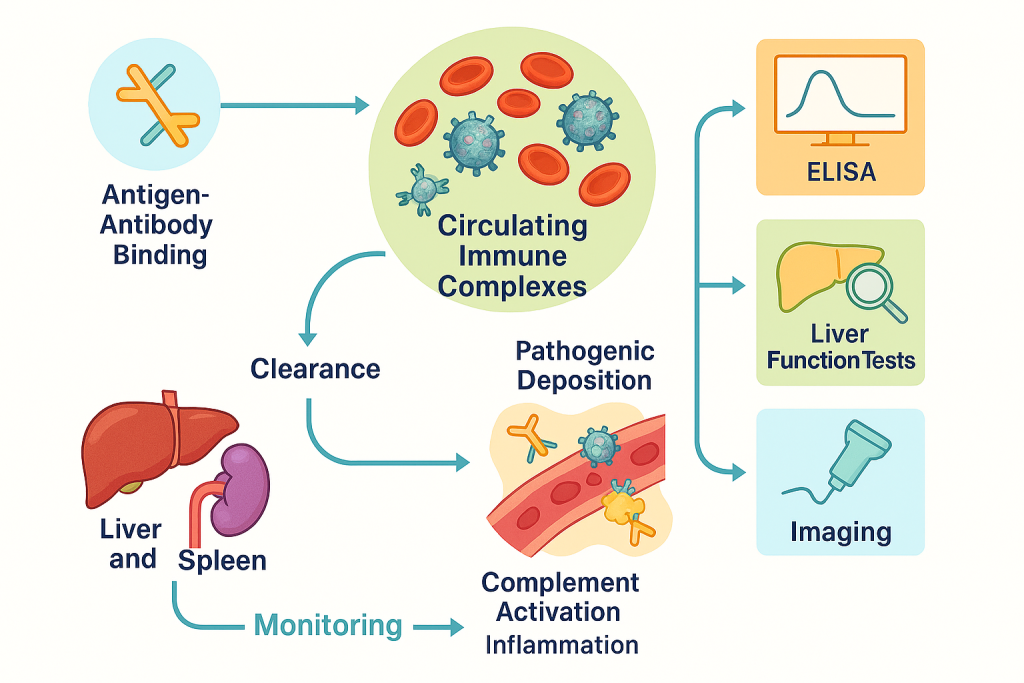
Circulating Immune Complexes are aggregates formed when antigens bind to antibodies in the bloodstream. Under normal physiological conditions, these complexes are cleared by the mononuclear phagocyte system, primarily in the liver and spleen. However, when clearance mechanisms are overwhelmed or impaired, CICs persist in circulation and deposit in tissues, triggering complement activation and inflammatory cascades.
Pathophysiological Role
CICs play a critical role in immune-mediated diseases. Their deposition in vascular endothelium, renal glomeruli, or hepatic tissue initiates local inflammation through complement fixation and recruitment of neutrophils. This process leads to tissue injury, fibrosis, and progressive organ dysfunction. In autoimmune liver diseases, CICs correlate with hepatocellular damage and immune-driven fibrosis, while in peptic ulcer disease, they contribute to mucosal immune dysregulation and chronic ulceration.
Clinical Significance
Monitoring CIC levels provides a dynamic marker of immune activity. Elevated CIC concentrations indicate active disease and predict exacerbations, making them valuable for risk stratification and therapeutic decision-making. Unlike static markers, CIC trends reflect real-time immunological changes, enabling clinicians to adjust therapy promptly.
Detection Methods
The most widely used technique for CIC detection is ELISA-based immunoassay, which offers high sensitivity and specificity. Other methods include polyethylene glycol precipitation, complement fixation assays, and immunofluorescence techniques for complex characterization. At CLRD, ELISA platforms are integrated with liver function tests and imaging for comprehensive evaluation.
Clinical Applications
CIC measurement is essential in autoimmune hepatitis, primary biliary cholangitis, and chronic peptic ulcer disease. It guides immunosuppressive therapy intensity, monitors treatment response, and predicts relapse risk. Incorporating CIC data into electronic health records allows longitudinal tracking and predictive analytics for personalized care.
CLRD’s Pioneering Role
The Center for Liver and Related Disorders (CLRD) was among the first institutions to integrate CIC detection into routine clinical practice for peptic ulcer and autoimmune liver diseases. This innovation provided a new dimension to disease assessment, moving beyond conventional biochemical markers to immunological profiling. By correlating CIC levels with disease severity and treatment response, CLRD enabled clinicians to stratify patients more accurately, anticipate complications, and tailor therapy to individual immunological burdens. This approach has transformed the management of chronic hepatic disorders and immune-mediated gastrointestinal conditions.
Diagnostic Capabilities
CLRD developed highly sensitive ELISA-based immunodiagnostic platforms for CIC quantification. These assays offer precise measurement of CIC concentrations, allowing dynamic monitoring throughout the disease course. Unlike traditional markers that often lag behind clinical changes, CIC levels provide real-time insights into immune activity. The integration of CIC data with liver function tests and imaging modalities creates a comprehensive diagnostic framework that supports early intervention and minimizes irreversible tissue damage. This capability is particularly valuable in autoimmune hepatitis and primary biliary cholangitis, where immune activity fluctuates and requires vigilant monitoring.
Treatment Specialization at CLRD
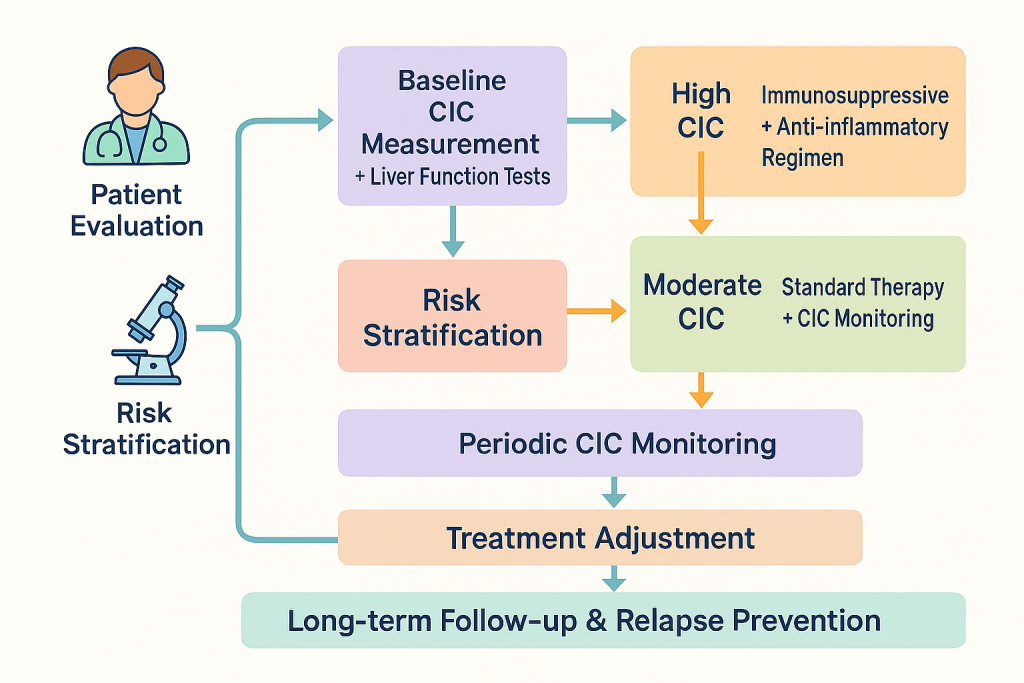
CIC monitoring is central to CLRD’s therapeutic protocols. Patients with high CIC loads are initiated on aggressive immunosuppressive regimens, including corticosteroids and azathioprine, to dampen immune-mediated injury. Those with moderate CIC levels receive standard therapy complemented by close immunological surveillance to prevent escalation. In peptic ulcer disease with immune-driven pathology, anti-inflammatory strategies and adjunctive antioxidant therapy are employed to mitigate oxidative stress associated with CIC deposition. This personalized approach ensures that treatment intensity matches immunological burden, reducing adverse effects and improving long-term outcomes.
CIC-Guided Treatment Pathway
The treatment pathway at CLRD begins with a comprehensive patient evaluation that includes clinical assessment and baseline laboratory investigations. Once the initial evaluation is complete, CIC measurement is performed alongside liver function tests to establish an immunological and biochemical profile. Based on these findings, patients are stratified into risk categories that determine the intensity of therapy. Individuals with markedly elevated CIC levels are started on aggressive immunosuppressive and anti-inflammatory regimens to control immune-mediated tissue damage, while those with moderate CIC concentrations receive standard therapy supplemented by close monitoring to prevent disease escalation. Throughout the treatment course, CIC levels are periodically reassessed to evaluate therapeutic response and guide adjustments in medication dosage or regimen. This dynamic monitoring ensures that therapy remains aligned with the patient’s immunological status, reducing the risk of relapse and minimizing unnecessary exposure to potent drugs. The pathway concludes with long-term follow-up, where CIC trends are integrated into predictive models for relapse prevention and sustained disease control.
Monitoring Frequency and Methods
Monitoring of circulating immune complexes at CLRD follows a structured protocol designed to capture dynamic changes in immune activity throughout the disease course. At baseline, CIC levels are measured during initial evaluation to establish an immunological profile. For patients with high CIC concentrations or active autoimmune liver disease, repeat testing is typically performed every two to four weeks during the induction phase of immunosuppressive therapy. This frequency ensures timely detection of therapeutic response and prevents uncontrolled immune-mediated injury. Once clinical stability is achieved and CIC levels decline, monitoring intervals are extended to every two to three months during maintenance therapy. In chronic hepatic disorders with fluctuating immune activity, additional testing may be warranted during suspected flares or prior to tapering immunosuppressive drugs.
The primary method employed at CLRD is an ELISA-based immunoassay, which offers high sensitivity and specificity for CIC quantification. This technique allows accurate measurement of antigen-antibody complexes in serum and is complemented by liver function tests and imaging studies for comprehensive assessment. In select cases, immune complex characterization using advanced techniques such as polyethylene glycol precipitation or complement fixation assays may be performed to evaluate pathogenic potential. All results are integrated into electronic health records, enabling longitudinal tracking and predictive analytics for relapse prevention.
Advantages of CIC-Based Treatment at CLRD
The CIC-based treatment model at CLRD offers several clinical advantages. First, it enables early detection of immune exacerbations, allowing timely therapeutic escalation before irreversible organ damage occurs. Second, it supports precision medicine by tailoring immunosuppressive therapy to individual immunological profiles, thereby minimizing drug toxicity and optimizing efficacy. Third, continuous CIC monitoring facilitates proactive relapse prevention, reducing hospitalization rates and improving quality of life. Finally, this approach enhances prognostic accuracy, empowering clinicians to counsel patients effectively regarding disease trajectory and treatment expectations.
CLRD’s Comprehensive Care Model
CLRD’s care model integrates diagnostics, therapeutics, and follow-up into a seamless continuum. Multidisciplinary teams comprising hepatologists, gastroenterologists, and immunologists collaborate to design individualized treatment plans. Advanced electronic health record systems capture CIC trends and generate predictive analytics, enabling clinicians to anticipate flares and adjust therapy preemptively. Patient education programs reinforce adherence and encourage early reporting of symptoms, ensuring sustained disease control. This holistic approach positions CLRD as a leader in immunologically informed care for complex hepatic and gastrointestinal disorders.
CLRD’s care model integrates diagnostics, therapeutics, and follow-up into a seamless continuum. Multidisciplinary teams comprising hepatologists, gastroenterologists, and immunologists collaborate to design individualized treatment plans. Advanced electronic health record systems capture CIC trends and generate predictive analytics, enabling clinicians to anticipate flares and adjust therapy preemptively. Patient education programs reinforce adherence and encourage early reporting of symptoms, ensuring sustained disease control. This holistic approach positions CLRD as a leader in immunologically informed care for complex hepatic and gastrointestinal disorders.
