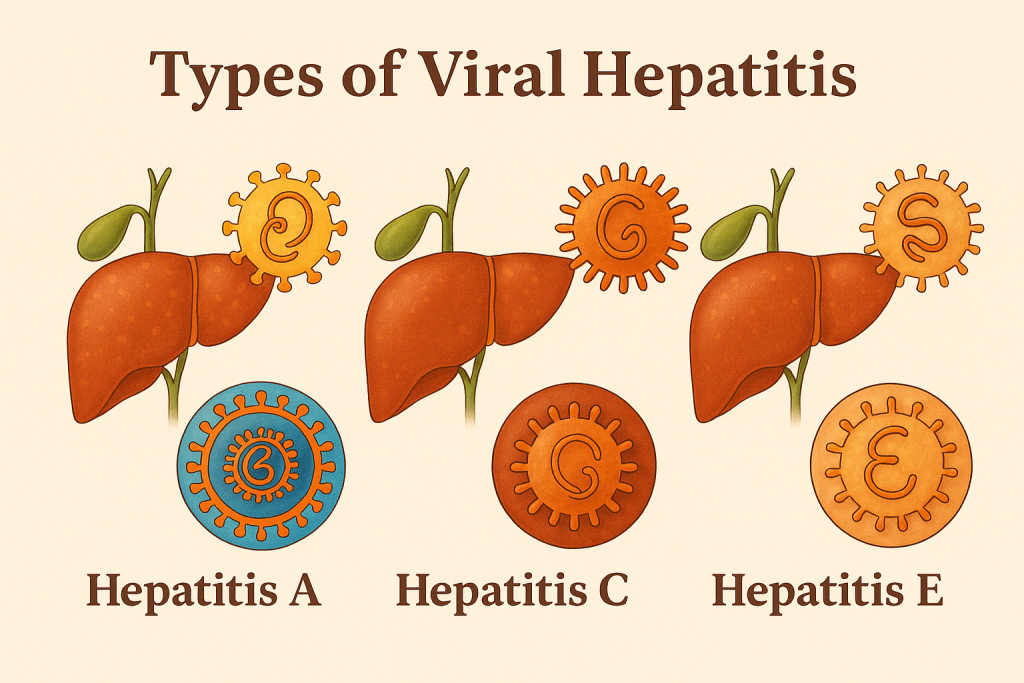
Viral Hepatitis (HBV, HCV, HEV)
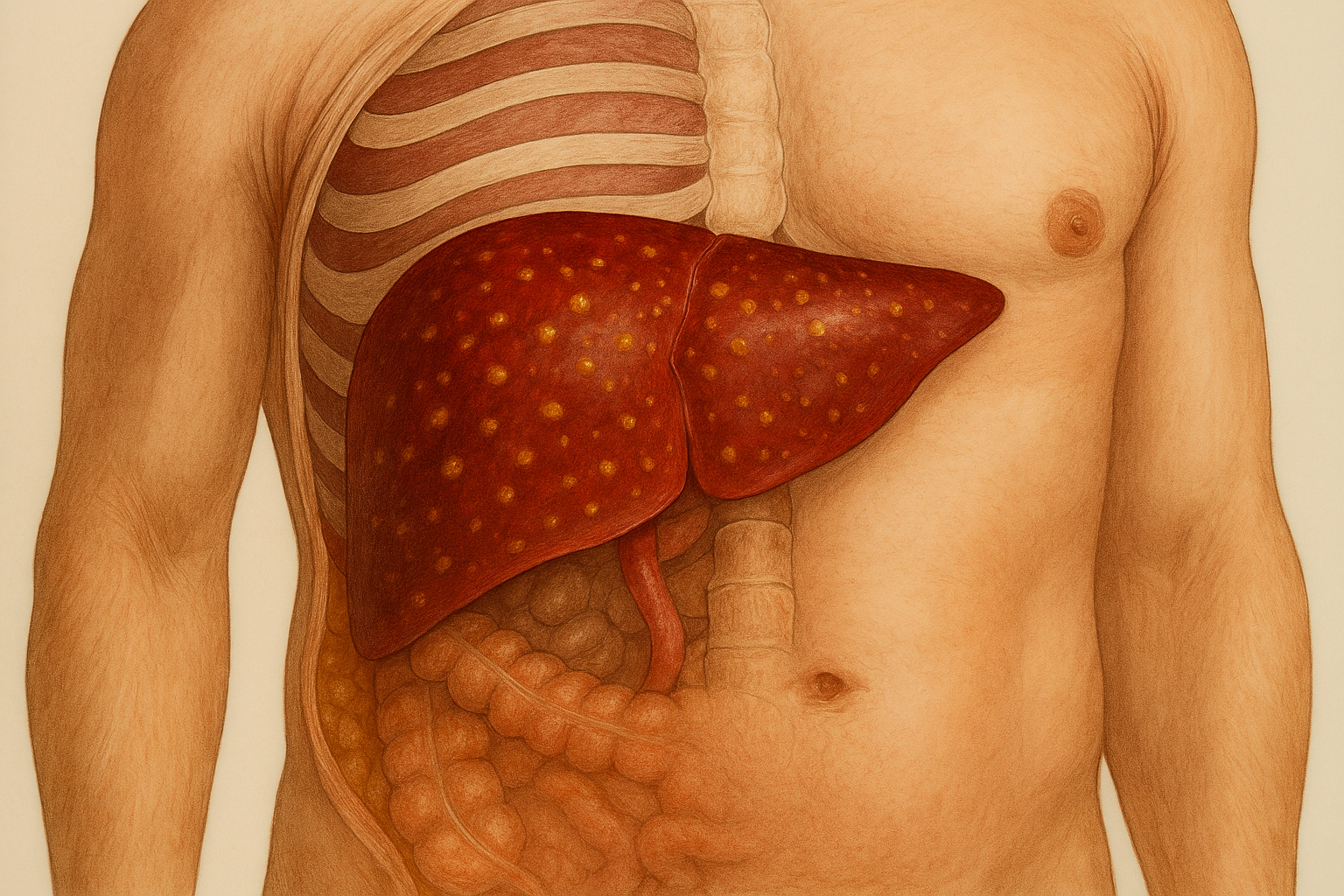
At CLRD, we recognize that a diagnosis of viral hepatitis can be life-altering. Our mission is to provide not just treatment, but a pathway to recovery and long-term wellness. With decades of pioneering research and clinical excellence, CLRD has become a trusted center for managing Hepatitis B, Hepatitis C, and Hepatitis E. Our approach is holistic and patient-focused, combining advanced diagnostics, personalized therapies, and compassionate care. We have successfully treated thousands of patients, helping them regain health and confidence. Whether you are newly diagnosed or living with chronic hepatitis, CLRD offers a comprehensive care model that prioritizes your well-being at every stage.
Hepatitis B (HBV)
CLRD offers comprehensive care for Hepatitis B, a viral infection that affects the liver and can lead to serious complications if left untreated. Our facility is equipped with advanced diagnostic tools that allow early detection of the virus, even in asymptomatic stages. We provide personalized treatment plans based on the patient’s viral load, liver function, and immune response. Our protocols include the use of potent antiviral medications that suppress viral replication and prevent liver damage. Patients are monitored regularly for treatment response, liver enzyme levels, and potential progression to cirrhosis or liver cancer. CLRD also offers specialized care for pregnant women and immunocompromised individuals, ensuring safe and effective management of HBV in complex cases.
Symptoms
Hepatitis B often begins subtly, with symptoms that can easily be mistaken for a common viral illness like the flu. In the early stages, many patients feel unusually tired, even after a full night’s sleep. This fatigue can interfere with daily activities and may be accompanied by a mild fever that comes and goes. Some individuals also experience aching joints, which may feel similar to arthritis or general body pain.
As the infection progresses, the liver begins to show signs of distress. One of the most noticeable symptoms is jaundice, which causes the skin and the whites of the eyes to turn yellow. This happens because the liver is unable to properly process bilirubin, a substance produced during the breakdown of red blood cells. When bilirubin builds up in the body, it leads to this yellow discoloration.
Patients may also feel a dull or sharp pain in the upper right side of the abdomen, where the liver is located. This discomfort can be persistent and may worsen after eating. Nausea and vomiting are common, and many patients lose their appetite, leading to unintended weight loss. These digestive symptoms are a result of the liver’s reduced ability to filter toxins and support digestion.
Another important sign is dark-colored urine, which may appear tea or cola-colored. This is due to excess bilirubin being excreted through the kidneys. At the same time, stools may become pale or clay-colored, indicating that bile flow from the liver is disrupted. Some patients also report itchy skin, which can be caused by bile salts accumulating in the bloodstream.
In many cases, especially when the infection becomes chronic, symptoms may be very mild or completely absent. This is why regular screening is crucial, particularly for individuals with a family history of hepatitis, those who have undergone blood transfusions, or people exposed to infected bodily fluids. At CLRD, we emphasize early detection and proactive care to prevent long-term liver damage and ensure a healthy recovery.
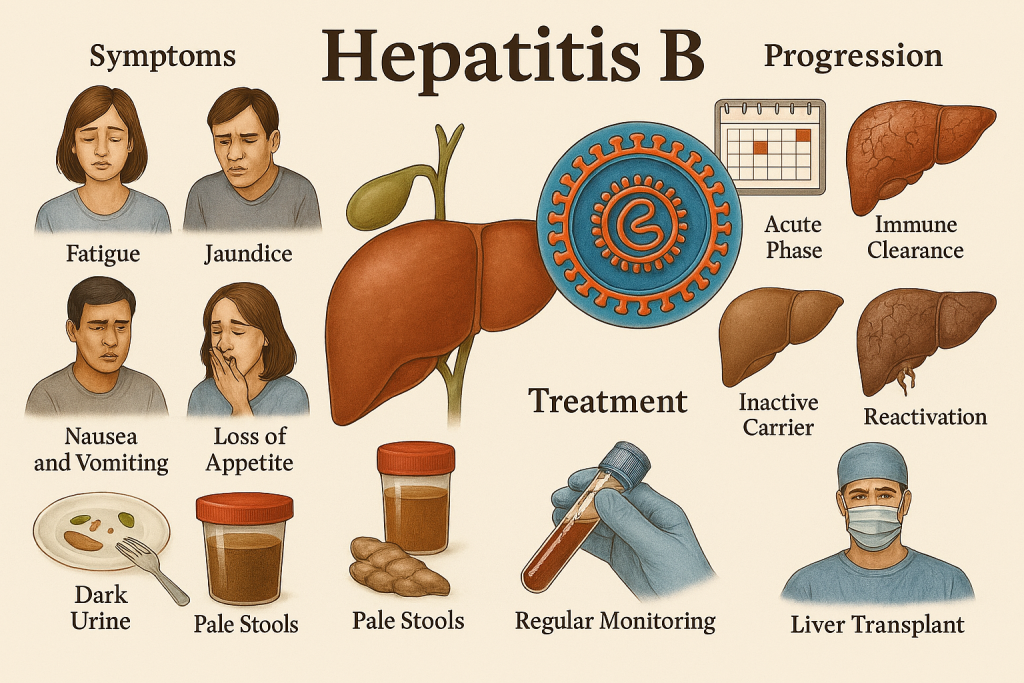
Stage-wise Progression
Hepatitis B progresses through several distinct stages, each affecting the liver differently and requiring specific medical attention. Understanding these stages helps patients and caregivers recognize the importance of early diagnosis and consistent monitoring.
1. Acute Phase:
This is the initial stage of infection, typically occurring within 1 to 4 months after exposure to the virus. During this phase, the virus begins to replicate in the liver. Some individuals may experience noticeable symptoms such as fever, fatigue, joint pain, nausea, and jaundice. However, many people remain asymptomatic, making it difficult to detect without screening. In some cases, the immune system successfully clears the virus on its own, leading to full recovery without long-term consequences.
2. Immune Clearance Phase:
If the virus is not cleared during the acute phase, the body enters a stage where the immune system actively tries to eliminate the virus. This immune response can cause inflammation in the liver, leading to elevated liver enzymes and potential liver cell damage. Patients may feel more fatigued during this phase, and symptoms like abdominal discomfort and jaundice may persist or worsen. This stage is critical, as ongoing inflammation can lead to scarring of liver tissue.
3. Inactive Carrier Phase:
In some individuals, the virus becomes less active after the immune system partially controls it. These patients are referred to as “inactive carriers.” The virus remains in the body but does not replicate aggressively, and liver damage is minimal or absent. Most people in this phase do not experience symptoms and may live without complications for years. However, regular monitoring is essential to detect any changes in viral activity or liver health.
4. Reactivation Phase:
In certain cases, the virus may become active again, especially if the immune system is weakened due to age, illness, or medications. This reactivation leads to renewed viral replication and liver inflammation. Patients may begin to experience symptoms again, and liver damage can accelerate. This phase increases the risk of developing liver fibrosis—a condition where healthy liver tissue is replaced by scar tissue.
5. Advanced Liver Disease:
If Hepatitis B remains untreated or poorly managed, it can progress to serious complications. Cirrhosis is a condition where extensive scarring disrupts liver function, leading to symptoms such as fluid retention, bleeding disorders, and confusion due to toxin buildup. Over time, cirrhosis may evolve into hepatocellular carcinoma (HCC), a form of liver cancer. At this stage, intensive treatment is required, and liver transplantation may be considered in severe cases.
At CLRD, we focus on identifying the disease early and intervening at every stage to prevent progression. Our personalized treatment plans, regular monitoring, and advanced diagnostics ensure that patients receive the best possible care to protect their liver and overall health.
Hepatitis C (HCV)
CLRD provides state-of-the-art treatment for Hepatitis C, a blood-borne viral infection that can silently damage the liver over years. Our expertise in genotyping Indian HCV strains allows us to tailor therapies to individual patients, ensuring optimal outcomes. We utilize Direct-Acting Antivirals (DAAs) that offer high cure rates with minimal side effects. Our team monitors patients closely throughout the treatment cycle, assessing viral load, liver function, and overall health. CLRD also manages complex cases, including those with co-infections or renal impairment, and provides post-treatment follow-up to prevent relapse and support liver regeneration.
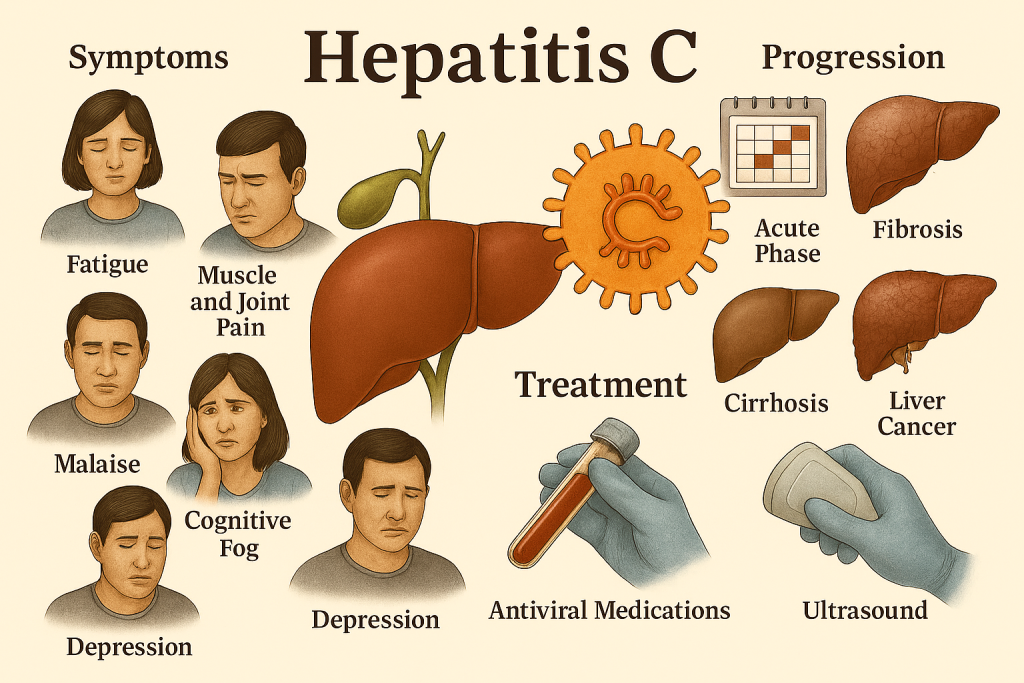
Symptoms
Hepatitis C is often called a “silent” infection because many people don’t feel sick when they first get it. In fact, during the early stages, most individuals have no symptoms at all. This means the virus can quietly live in the body and slowly damage the liver over many years without the person even knowing it. That’s why regular screening is so important, especially for people who may have been exposed to infected blood or medical procedures in the past.
When symptoms do begin to appear, they are usually vague and easy to overlook. One of the most common signs is persistent fatigue—a deep tiredness that doesn’t go away even after rest. People may feel drained and struggle to keep up with daily tasks. Muscle and joint pain can also occur, often resembling the aches of a mild flu or arthritis.
Some patients report feeling a general sense of malaise, which means they just don’t feel well but can’t pinpoint exactly why. This can be accompanied by cognitive fog, where thinking feels slower, memory is affected, and concentration becomes difficult. In some cases, depression may develop, adding to the emotional and physical burden of the disease.
As Hepatitis C progresses and the liver becomes more damaged, more serious symptoms begin to show. Jaundice may develop, causing the skin and eyes to turn yellow. This happens because the liver can no longer properly process waste products in the blood. Patients may also notice easy bruising or bleeding, which is a sign that the liver is struggling to produce the proteins needed for blood clotting.
Other symptoms in advanced stages may include swelling in the legs or abdomen, itchy skin, and dark-colored urine. These signs indicate that the liver is under significant stress and that medical attention is urgently needed.
At CLRD, we encourage early testing and offer comprehensive care to manage symptoms, prevent liver damage, and improve quality of life. Our goal is to detect Hepatitis C before it causes serious harm and to guide patients through a safe and effective treatment journey.
Stage-wise Progression
Hepatitis C is a slow-progressing viral infection that primarily affects the liver. At CLRD, we understand that the disease often begins silently, with no symptoms, and can remain undetected for years. This silent nature makes early diagnosis and intervention critical.
The acute phase of Hepatitis C occurs within six months of exposure. During this time, the virus enters the bloodstream and begins to replicate in the liver. Most individuals do not experience noticeable symptoms, although some may report mild fatigue, fever, or abdominal discomfort. In rare cases, jaundice may appear. The immune system may clear the virus naturally in a small percentage of patients, but in most cases, the infection becomes chronic.
In the chronic phase, the virus continues to replicate, causing gradual damage to liver cells. This phase can last for decades without overt symptoms, but internally, the liver undergoes inflammation and scarring. Patients may begin to experience persistent fatigue, joint pain, and cognitive issues such as brain fog or depression. As the liver becomes increasingly compromised, symptoms like jaundice, easy bruising, and swelling in the legs or abdomen may emerge.
The next stage is fibrosis, where scar tissue begins to replace healthy liver tissue. This process is slow but progressive, and without treatment, it leads to cirrhosis, a condition marked by extensive scarring and impaired liver function. Cirrhosis can result in complications such as portal hypertension, ascites, and hepatic encephalopathy.
In the end-stage, patients may develop hepatocellular carcinoma (liver cancer) or liver failure, both of which require intensive care and may necessitate liver transplantation. CLRD’s early intervention strategies, including genotype-specific antiviral therapy, aim to halt this progression and restore liver health before irreversible damage occurs.
Hepatitis E (HEV)
CLRD offers expert care for Hepatitis E, a waterborne viral infection that primarily affects the liver. Our diagnostic capabilities include rapid PCR-based detection, allowing timely intervention. While most HEV cases are self-limiting, CLRD provides specialized care for high-risk groups such as pregnant women and immunocompromised patients. Our treatment protocols focus on supportive care, hydration, and monitoring of liver function. During outbreaks, CLRD plays a key role in public health response, offering screening, education, and preventive strategies.
Symptoms
Hepatitis E is a viral infection that primarily affects the liver and is usually spread through contaminated water. The symptoms often begin suddenly and can resemble those of a common flu, which makes it easy to overlook in the early stages.
Most patients first notice a fever, which may be mild or moderate, accompanied by a feeling of extreme tiredness or exhaustion. This fatigue can be persistent and may interfere with daily activities, even simple tasks like walking or eating. As the infection progresses, many individuals experience nausea, a sensation of queasiness or an urge to vomit, which may be followed by actual vomiting. These digestive symptoms are often accompanied by abdominal pain, especially in the upper right side of the abdomen where the liver is located. This pain may feel like a dull ache or pressure and can worsen after meals.
One of the most recognizable signs of Hepatitis E is jaundice, which causes the skin and the whites of the eyes to turn yellow. This happens because the liver, which normally helps remove waste from the body, becomes inflamed and cannot process bilirubin properly. Alongside jaundice, patients may notice dark-colored urine, which may appear tea or cola-like, and pale or clay-colored stools, both of which are signs that the liver is not functioning normally. In some cases, the liver may become enlarged, which can be felt as a swelling or fullness in the upper abdomen.
For most healthy individuals, these symptoms gradually improve within a few weeks, and the liver returns to normal without long-term damage. However, in vulnerable populations, such as pregnant women, especially during the third trimester, or people with weakened immune systems, Hepatitis E can become severe. In these cases, the infection may lead to acute liver failure, which is a life-threatening condition requiring immediate medical care.
At CLRD, we provide timely diagnosis and supportive care to help patients recover safely. Our team closely monitors liver function and symptoms, especially in high-risk groups, to prevent complications and ensure a smooth recovery.

Stage-wise Progression
Hepatitis E usually follows a short-term course, but its progression can vary depending on the patient’s overall health and immune status. At CLRD, we help patients understand each stage of the infection so they can receive timely care and avoid complications.
1. Acute Phase:
This is the initial stage of Hepatitis E and typically begins 2 to 8 weeks after exposure to the virus, often through contaminated water or food. During this phase, the virus starts to multiply in the liver, and symptoms such as fever, fatigue, nausea, vomiting, and jaundice begin to appear. Most healthy individuals recover fully within a few weeks without any long-term damage to the liver. The body’s immune system fights off the virus, and liver function gradually returns to normal. Supportive care, including rest, hydration, and a balanced diet, is usually sufficient during this phase.
2. Severe Acute Phase in Pregnant Women:
While most people recover easily, pregnant women, especially those in their third trimester, are at a much higher risk of developing a severe form of Hepatitis E known as fulminant hepatitis. This is a rapid and dangerous deterioration of liver function that can lead to liver failure and, in some cases, death. Symptoms may escalate quickly, including intense jaundice, confusion, bleeding, and fluid accumulation. At CLRD, we provide specialized monitoring and emergency care for pregnant women with HEV to protect both maternal and fetal health.
3. Chronic Phase in Immunocompromised Patients:
In individuals with weakened immune systems, such as those undergoing chemotherapy, organ transplant recipients, or patients with HIV, the virus may not be cleared effectively. Instead of resolving, Hepatitis E can become chronic, meaning the virus continues to live in the liver and cause ongoing inflammation. This persistent infection can slowly damage the liver over time, increasing the risk of fibrosis and cirrhosis. CLRD offers advanced antiviral therapies and regular liver function monitoring to manage chronic HEV and prevent long-term complications.
By understanding these stages, patients and caregivers can recognize when symptoms are mild and self-limiting, and when they require urgent medical attention. CLRD’s expert team ensures that every patient receives the right care at the right time, tailored to their individual health needs.
At CLRD, our commitment to excellence in liver care is reflected in our comprehensive approach to managing Hepatitis B, Hepatitis C, and Hepatitis E. Each type of viral hepatitis presents unique challenges, but with decades of research-backed protocols and patient-centered treatment strategies, we have successfully guided thousands toward recovery. From early detection and personalized antiviral therapies to specialized care for vulnerable populations, our team ensures that every patient receives timely, effective, and compassionate support. Whether the infection is acute, chronic, or complex, CLRD stands as a trusted center for healing, prevention, and long-term liver health. We believe that with the right care, every patient has the potential to overcome hepatitis and reclaim a healthy life.
