Hepatocellular Carcinoma (HCC)
At CLRD, we recognize that a diagnosis of liver cancer can feel overwhelming. Our mission is to transform that fear into hope through early detection, advanced treatment, and compassionate care. For decades, CLRD has been at the forefront of hepatology and oncology research, pioneering innovations that have redefined liver cancer management. Every patient is unique, and so is our approach, personalized, research-driven, and focused on restoring health and quality of life.

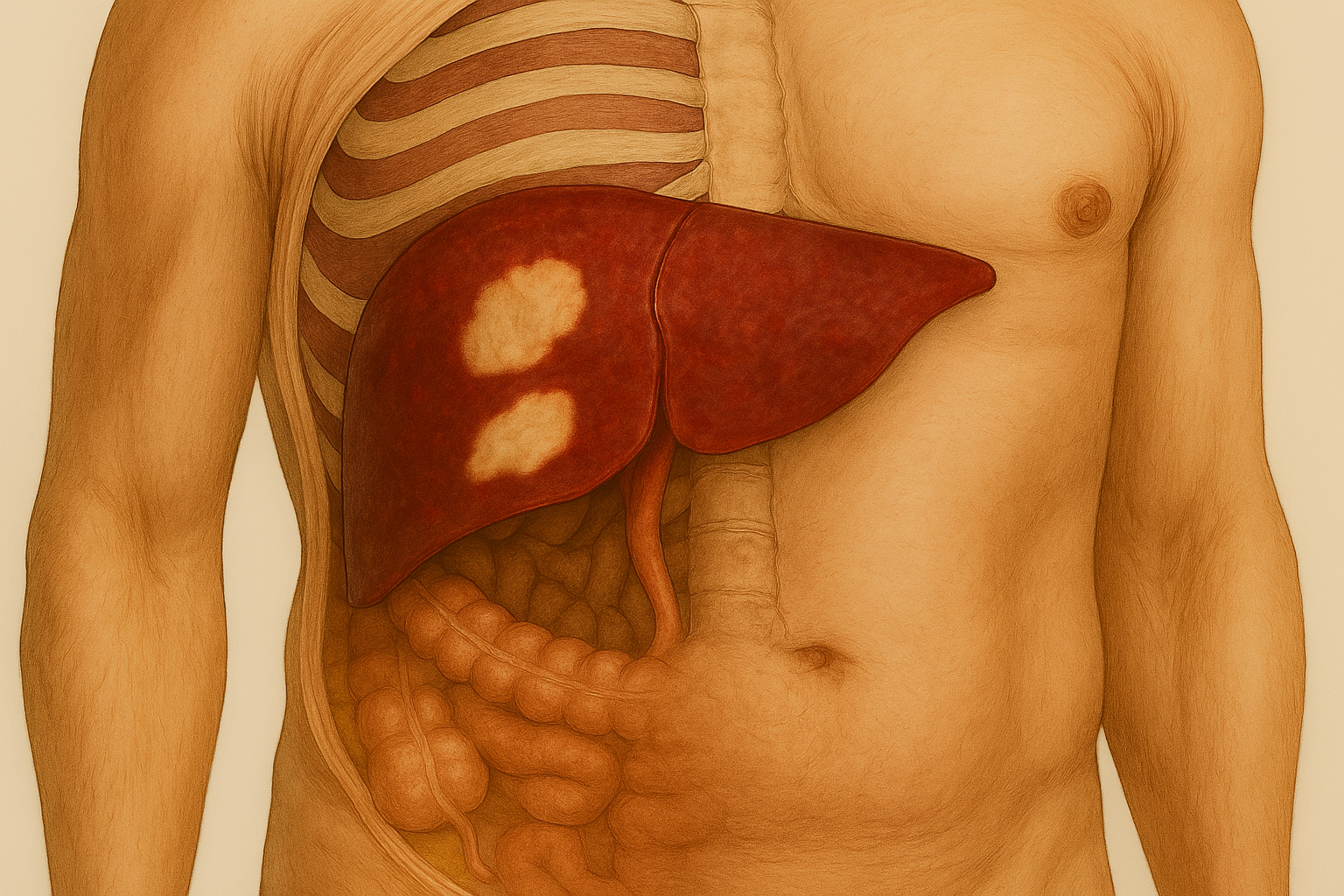
Hepatocellular carcinoma is the most common primary liver cancer, accounting for nearly 80–90% of all liver malignancies worldwide. It typically arises in the setting of chronic liver disease, such as hepatitis B or C infection, alcoholic liver disease, or non-alcoholic fatty liver disease. At CLRD, our understanding of HCC is rooted in decades of pioneering research and clinical practice, enabling us to detect and treat this condition at its earliest stages.
Etiology and Risk Factors
HCC develops when chronic liver injury leads to cirrhosis and genetic alterations in hepatocytes. CLRD’s early studies on hepatitis B surface antigen prevalence (Hepatology, 1982) and delta infection (Hepatology Letters, 1987) highlighted viral hepatitis as a major contributor to liver cancer in India. Our investigations into occupational hazards, such as liver damage among insecticide sprayers (Proceedings of International Symposium, 1984), further expanded the understanding of environmental risk factors.
Pathogenesis and Molecular Insights
The progression from chronic liver disease to HCC involves complex genetic and epigenetic changes. CLRD has extensively studied these mechanisms, including:
- Alpha-fetoprotein (AFP) as a Biomarker: Our landmark publication on AFP in hepatomas (Indian Journal of Pathology and Microbiology, 1980) established AFP as a cornerstone for early HCC detection.
- Genetic Polymorphisms and Molecular Pathways: Research spanning decades has explored variations in genes such as XRCC-1 and APE-1, contributing to cancer susceptibility (Inflammation Research, 2012).
- Epigenetic Regulation: Studies on DNA methylation patterns in gastric and hepatic malignancies (Journal of Clinical Laboratory Analysis, 2009) provided insights into tumor biology.
Diagnostic Advances
CLRD integrates imaging modalities with molecular diagnostics for accurate detection. Our work on liver scanning techniques (Journal of Association of Physicians of India, 1977) laid the foundation for modern imaging protocols. Today, we combine high-resolution imaging with AFP screening and next-generation sequencing for comprehensive tumor profiling.
Innovations in Therapy
Our commitment to translational research has led to breakthroughs in targeted therapy:
- Nanotechnology-Based Drug Delivery: Development of sorafenib-gold nanoconjugates to overcome drug resistance in hepatoblastoma cells (Scientific Reports, 2017).
- Stem Cell-Derived Exosomes: Leveraging regenerative medicine to support liver function during cancer treatment (World Journal of Stem Cells, 2015).
- Bioengineered Liver Constructs: Creating humanized livers for drug testing and supportive therapy (World Journal of Hepatology, 2018).
These innovations ensure that patients at CLRD receive therapies that are not only effective but also minimize systemic toxicity.
Symptoms
HCC often begins silently, which makes early detection challenging. Many patients do not experience noticeable symptoms until the disease has progressed significantly. At CLRD, we emphasize proactive screening for high-risk individuals because subtle signs can easily be overlooked.
Early Stage Symptoms
- Mild fatigue and general weakness that persists despite rest.
- Slight discomfort or fullness in the upper right abdomen.
- Occasional nausea or reduced appetite.
Progressive Symptoms As the tumor grows or multiple nodules develop, symptoms become more pronounced:
- Unexplained Weight Loss: A sudden drop in weight without changes in diet or exercise.
- Persistent Abdominal Pain: Pain or pressure in the upper right quadrant, sometimes radiating to the back or shoulder.
- Digestive Changes: Loss of appetite, bloating, and early satiety.
Advanced Stage Symptoms When HCC invades blood vessels or spreads beyond the liver:
- Jaundice: Yellowing of the skin and eyes due to impaired liver function.
- Ascites: Fluid accumulation in the abdomen causing swelling and discomfort.
- Severe Fatigue: Extreme tiredness that interferes with daily activities.
- Systemic Symptoms: Fever, muscle wasting, and signs of liver failure such as confusion or bleeding tendencies.
Why These Symptoms Matter Many of these symptoms overlap with other liver conditions, making accurate diagnosis essential. CLRD uses a combination of imaging, alpha-fetoprotein (AFP) testing, and molecular profiling to confirm HCC early, often before severe symptoms appear.

Stage-wise Progression
HCC does not develop overnight—it evolves through distinct stages, each with unique clinical features and treatment implications. Understanding these stages helps patients and caregivers anticipate what lies ahead and make informed decisions.
Stage 1: Early Stage (Localized Tumor)
- Clinical Features: Tumors are small (usually <2 cm) and confined to the liver without vascular invasion. Most patients are asymptomatic.
- Detection: Often discovered during routine screening in high-risk individuals using imaging and alpha-fetoprotein (AFP) testing.
- CLRD Approach: Our early detection protocols, supported by decades of AFP research (Indian Journal of Pathology and Microbiology, 1980), enable timely intervention. Surgical resection or ablation offers excellent outcomes at this stage.
Stage 2: Intermediate Stage
- Clinical Features: Tumors increase in size or multiple nodules appear. Mild symptoms such as fatigue, abdominal discomfort, and reduced appetite become noticeable.
- Disease Dynamics: Liver function remains relatively preserved, but tumor burden is significant.
- CLRD Approach: We employ transarterial chemoembolization (TACE) and radiofrequency ablation (RFA) to control tumor growth. Molecular profiling guides targeted therapy for optimal results.
Stage 3: Advanced Stage
- Clinical Features: Tumor invades major blood vessels (portal vein or hepatic vein) or spreads beyond the liver. Symptoms include severe pain, jaundice, ascites, and systemic weakness.
- Disease Dynamics: Liver function deteriorates, and complications such as portal hypertension and bleeding risk increase.
- CLRD Approach: Our integrated oncology-hepatology model combines systemic therapy, immunotherapy, and nanoconjugate-based drug delivery (Scientific Reports, 2017) to manage disease progression and improve survival.
Stage 4: End Stage
- Clinical Features: Extensive liver damage, metastasis to distant organs, and signs of liver failure such as confusion, bleeding tendencies, and cachexia.
- CLRD Approach: At this stage, our focus shifts to palliative care and quality of life. We also explore regenerative options using hepatic stem cells (World Journal of Stem Cells, 2015) to support liver function where feasible.
Why This Matters: Each stage demands a different therapeutic strategy. CLRD’s strength lies in tailoring treatment plans based on stage, liver function, and molecular profile—ensuring patients receive the most effective care at every step.
Our Treatment Capabilities
CLRD offers a full spectrum of treatment options, tailored to each patient’s condition:
1. Surgical Excellence
Liver Resection: For localized tumors in patients with adequate liver function.
Liver Transplantation: For advanced cases with cirrhosis, supported by comprehensive pre- and post-transplant care.
2. Targeted Therapies Our research has led to breakthroughs in nanoconjugate-based drug delivery and stem cell-derived exosome therapy, enabling precise targeting of cancer cells while minimizing side effects.
3. Interventional Oncology
Transarterial Chemoembolization (TACE): Blocks blood supply to the tumor while delivering chemotherapy directly.
Radiofrequency Ablation (RFA): Destroys cancer cells using heat energy.
4. Systemic and Immunotherapy We integrate molecular-targeted drugs and immunotherapy based on genetic and epigenetic profiling, ensuring personalized treatment strategies.
5. Regenerative Medicine Leveraging decades of stem cell research, CLRD supports liver regeneration in select cases, improving long-term outcomes.
Research Legacy
CLRD’s pioneering work in HCC includes:
- Alpha-fetoprotein Studies: Early publications (Indian Journal of Pathology and Microbiology, 1980) established AFP as a key biomarker for hepatomas.
- Genetic and Epigenetic Insights: Continuous research into molecular pathways influencing HCC progression.
- Nanotechnology Innovations: Development of sorafenib-gold nanoconjugates for reversing drug resistance (Scientific Reports, 2017).
- Stem Cell Applications: Hepatic stem cell transplantation for cirrhosis and liver failure (World Journal of Stem Cells, 2015).
These contributions have shaped global understanding of liver cancer and positioned CLRD as a leader in advanced hepatology care.
