Chronic Liver Disease (CLD)
At the Center for Liver Research and Diagnostics (CLRD), we understand that chronic liver disease is not just a medical condition, it’s a life-altering challenge that affects every aspect of a patient’s well-being. Our approach is deeply patient-centric, combining cutting-edge diagnostics, personalized pharmacotherapy, and pioneering regenerative medicine to restore liver health and improve quality of life. With decades of research-backed expertise, CLRD has successfully treated thousands of CLD cases using customized care plans that include lifestyle interventions, antiviral therapies, and cellular therapies. Our multidisciplinary team ensures that each patient receives holistic care tailored to their unique condition and progression stage.

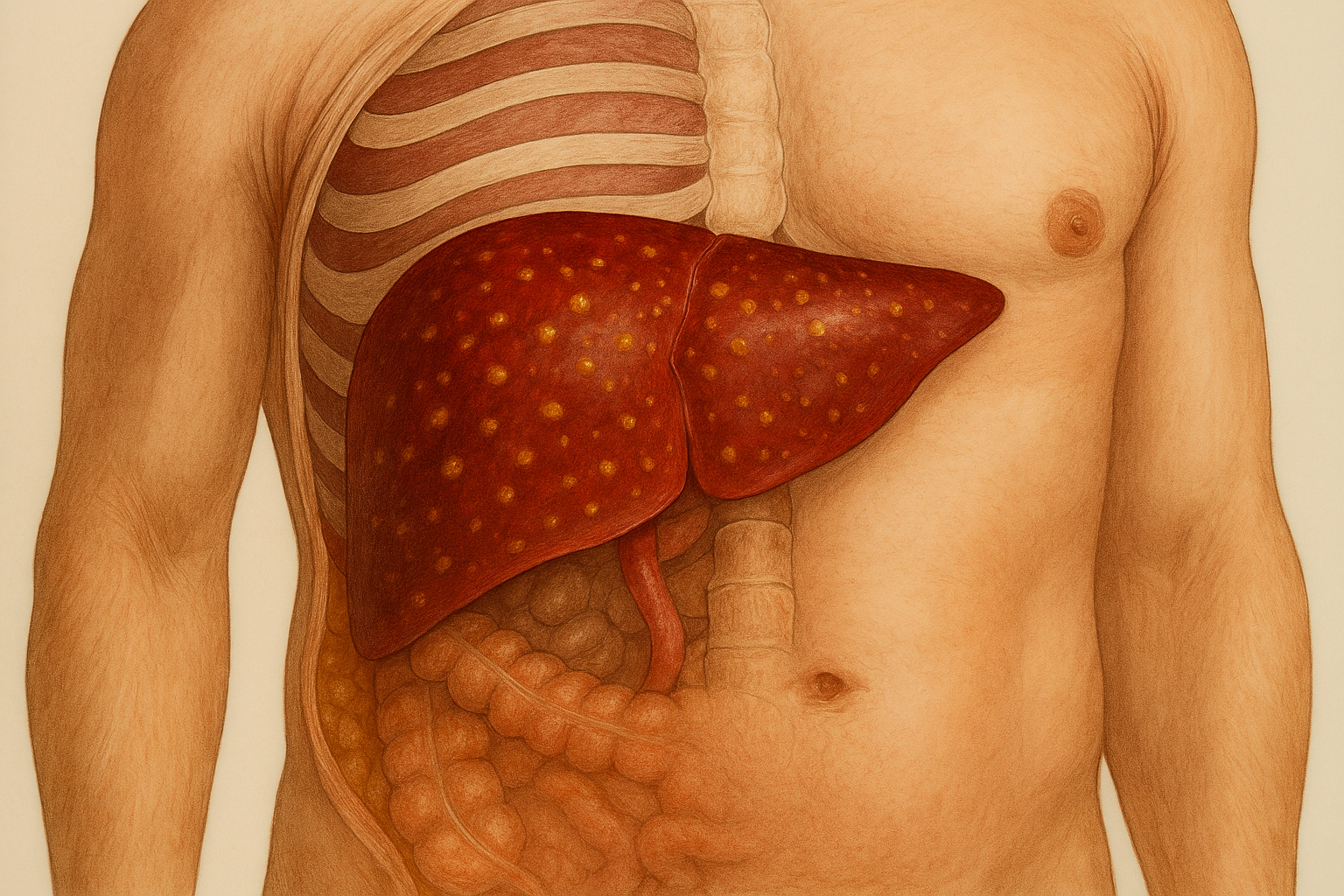
Alpha-1-Antitrypsin Deficiency-Related Liver Disease
Alpha-1-antitrypsin (AAT) deficiency is a genetic disorder that affects the production of a protein responsible for protecting tissues from inflammation-related damage. While it is commonly associated with lung disease, it can also lead to serious liver complications. At CLRD, we recognize the liver-specific impact of this condition and have developed specialized protocols to diagnose and treat it effectively.
Symptoms
Patients with liver involvement due to AAT deficiency may experience:
- Persistent fatigue: Feeling tired even after adequate rest.
- Jaundice: Yellowing of the skin and eyes due to impaired bilirubin processing.
- Elevated liver enzymes: Often detected during routine blood tests, indicating liver stress.
- Abdominal discomfort: Especially in the upper right quadrant, where the liver is located.
- Hepatomegaly: Enlargement of the liver, which may be felt as fullness or pressure.
These symptoms may vary in intensity and often go unnoticed in early stages, making timely diagnosis crucial.
Stage-wise Progression
CLRD has been at the forefront of identifying and managing liver disease caused by AAT deficiency. Our approach includes:
Early Detection
Using advanced genetic and biochemical screening, we identify AAT deficiency before significant liver damage occurs.Customized Pharmacotherapy
Patients receive enzyme replacement therapy and medications to reduce liver inflammation and prevent progression.Regenerative Medicine
CLRD has successfully implemented stem cell-based therapies, particularly using hepatic progenitor cells, to support liver regeneration. These cells help restore damaged liver tissue and improve overall liver function.Long-Term Monitoring and Support
Patients are enrolled in personalized care plans that include regular liver function monitoring, nutritional guidance, and lifestyle modifications to reduce liver stress.
Through these interventions, CLRD has helped numerous patients stabilize their condition, avoid liver transplantation, and lead healthier lives.
Our Treatment Capabilities
Early Stage
The disease may be silent, with only mild abnormalities in liver function tests. Patients are usually asymptomatic, and the condition is often discovered incidentally.Intermediate Stage
Inflammation begins to damage liver cells. Fibrosis (scarring) starts forming, and symptoms like fatigue and mild jaundice may appear. Liver function may start to decline.Advanced Stage
Extensive fibrosis leads to cirrhosis, a condition where normal liver tissue is replaced by scar tissue. This stage carries a high risk of complications such as portal hypertension and hepatocellular carcinoma (liver cancer).
Alcoholic Liver Disease (ALD)
Alcoholic Liver Disease (ALD) is a progressive condition caused by excessive and prolonged alcohol consumption. It affects the liver’s ability to function properly and can lead to irreversible damage if not addressed early. At CLRD, we understand the physical, emotional, and social challenges faced by individuals with ALD. Our care model is designed to support patients through every stage of recovery, starting from diagnosis to complete liver rehabilitation.

Symptoms
The symptoms of ALD can vary depending on the severity and duration of alcohol use. Common signs include:
- Fatigue and weakness: A constant feeling of tiredness due to reduced liver efficiency.
- Loss of appetite: Often accompanied by weight loss and nutritional deficiencies.
- Nausea and vomiting: Especially after meals or alcohol consumption.
- Jaundice: Yellowing of the skin and eyes, indicating liver dysfunction.
- Abdominal pain and swelling: Caused by inflammation or fluid buildup (ascites).
These symptoms may worsen over time and can significantly affect daily life and overall well-being.
Stage-wise Progression
Fatty Liver (Steatosis)
This is the earliest stage where fat accumulates in liver cells. It is usually reversible with complete abstinence from alcohol and lifestyle changes. Most patients are asymptomatic at this stage.Alcoholic Hepatitis
In this stage, the liver becomes inflamed. Patients may experience fever, jaundice, and abdominal pain. Liver function begins to decline, and the risk of complications increases.Cirrhosis
This is the most advanced stage, where healthy liver tissue is replaced by scar tissue. Cirrhosis is irreversible and can lead to liver failure, internal bleeding, and increased risk of liver cancer.
Our Treatment Capabilities
CLRD has conducted extensive research on liver damage caused by chronic alcohol consumption, including studies on regional practices such as Gudumba (illicit alcohol) consumption. Our treatment approach includes:
- Comprehensive Detoxification Programs
Patients undergo medically supervised detox to safely eliminate alcohol from the body, reducing withdrawal symptoms and preventing further liver damage. - Nutritional and Lifestyle Counseling
Our team provides personalized dietary plans and behavioral support to help patients maintain sobriety and improve liver health. - Pharmacological Support
Medications are prescribed to manage inflammation, prevent complications, and support liver function. - Regenerative Therapies
CLRD has successfully used stem cell transplantation, particularly hepatic progenitor cells, to regenerate damaged liver tissue in patients with advanced ALD. These therapies have shown significant improvement in liver function and quality of life. - Long-Term Monitoring and Rehabilitation
Patients receive ongoing care, including regular liver function tests, psychological support, and relapse prevention strategies.
CLRD’s holistic and compassionate approach has helped many individuals recover from ALD, avoid liver transplantation, and rebuild their lives with renewed health and hope.
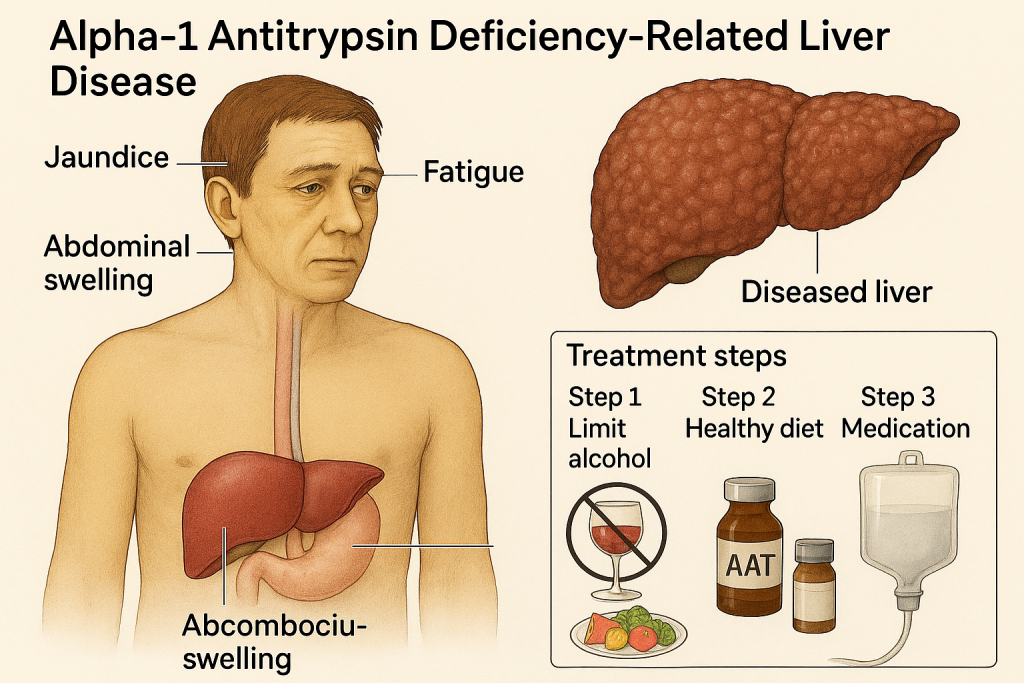
Liver Damage Due to Environmental Toxins
Liver damage caused by environmental toxins is a serious and often overlooked health issue. Exposure to harmful chemicals, such as pesticides, industrial solvents, and heavy metals, can silently impair liver function over time. At CLRD, we have extensively studied the impact of occupational and environmental exposures on liver health, particularly among agricultural workers and industrial laborers. Our expertise allows us to diagnose toxin-induced liver disease early and offer effective, personalized treatment strategies.
Symptoms
The symptoms of toxin-related liver damage may develop gradually and can include:
- Persistent fatigue: A constant feeling of tiredness due to impaired detoxification.
- Skin changes: Itching, rashes, or discoloration caused by toxin buildup.
- Abnormal liver function tests: Elevated enzymes without obvious cause.
- Digestive issues: Nausea, bloating, and loss of appetite.
- Neurological symptoms: Confusion or memory issues in advanced cases due to hepatic encephalopathy.
These symptoms may be subtle initially but can worsen with continued exposure or delayed diagnosis.
Stage-wise Progression
Initial Exposure
The liver begins to show signs of stress, often reflected in mildly elevated liver enzymes. Patients may not feel any symptoms at this stage.Chronic Exposure
Continued contact with toxins leads to inflammation and fibrosis. Symptoms like fatigue, skin irritation, and digestive discomfort become more noticeable.Advanced Toxicity
Extensive liver damage results in cirrhosis, portal hypertension, and potential liver failure. Patients may experience severe complications, including fluid accumulation and bleeding disorders.
Our Treatment Capabilities
CLRD has been a pioneer in identifying and managing liver damage caused by environmental toxins. Our research includes landmark studies on grape sprayers and insecticide handlers, revealing the occupational hazards linked to liver disease. Based on this expertise, our treatment approach includes:
- Advanced Diagnostic Screening
We use specialized tests to detect toxin-related liver damage early, even before symptoms appear. This includes liver imaging, enzyme profiling, and exposure history analysis. - Detoxification Protocols
Patients undergo medically supervised detox programs to eliminate harmful substances from the body. These protocols are tailored to the type and duration of exposure. - Antioxidant and Supportive Therapy
CLRD provides targeted antioxidant treatments to reduce oxidative stress and support liver cell recovery. Nutritional supplements and liver-protective medications are also prescribed. - Regenerative Medicine
In cases of advanced damage, stem cell therapy using hepatic progenitor cells and fetal hepatocytes is employed to regenerate liver tissue. These therapies have shown remarkable success in restoring liver function and preventing progression to liver failure. - Occupational Health Counseling
Patients receive guidance on avoiding further exposure, including protective measures and lifestyle adjustments. We also collaborate with public health agencies to raise awareness about environmental liver risks.
CLRD’s integrated approach has helped numerous patients recover from toxin-induced liver damage, regain liver function, and avoid long-term complications. Our commitment to early detection and innovative therapies ensures that patients receive the best possible care.
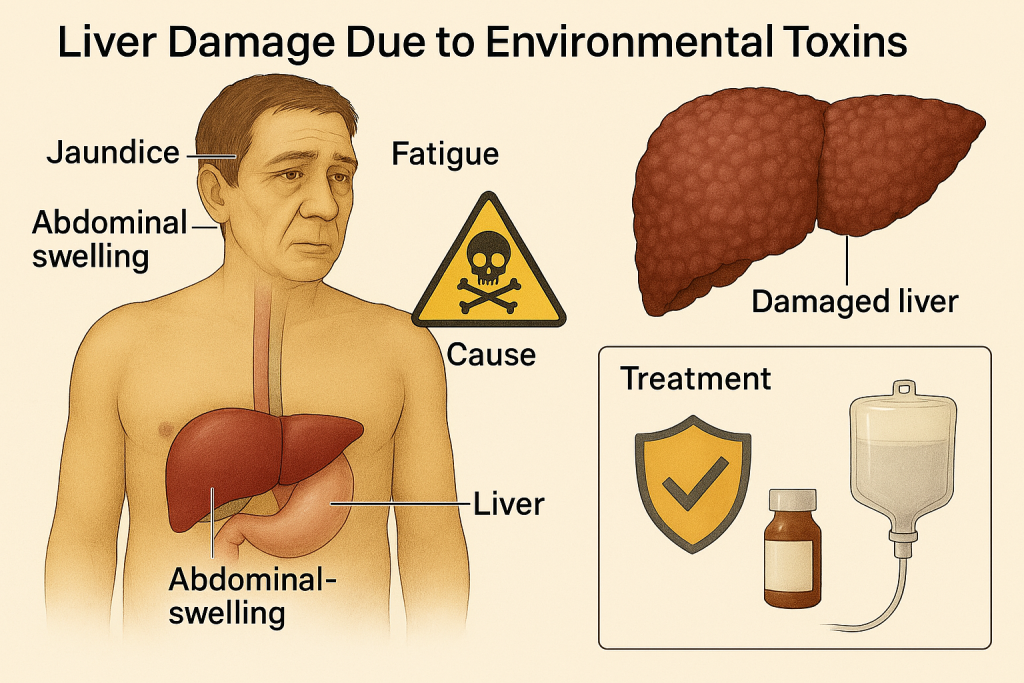
Viral Hepatitis-Induced Chronic Liver Disease (HBV, HCV)
Viral hepatitis is a major cause of chronic liver disease worldwide. Hepatitis B (HBV) and Hepatitis C (HCV) are viral infections that can silently damage the liver over years, leading to fibrosis, cirrhosis, and even liver cancer. At CLRD, we have decades of experience in diagnosing, managing, and treating viral hepatitis. Our approach combines advanced diagnostics, personalized antiviral therapy, and regenerative medicine to restore liver health and prevent complications.
Symptoms
The symptoms of chronic viral hepatitis may be mild or absent in early stages, but can include:
- Jaundice: Yellowing of the skin and eyes due to impaired bilirubin processing.
- Dark urine and pale stools: Indicating bile flow disruption.
- Fatigue: Persistent tiredness due to liver dysfunction.
- Abdominal pain: Especially in the upper right side.
- Joint pain and fever: More common in HBV-related cases.
- Loss of appetite and nausea
These symptoms may fluctuate and often go unnoticed until the disease has progressed significantly.
Stage-wise Progression
Acute Infection
The virus enters the body and may cause flu-like symptoms or mild jaundice. In some cases, the infection resolves on its own.Chronic Hepatitis
If the virus persists for more than six months, it becomes chronic. The liver undergoes slow, ongoing inflammation and damage. Patients may remain asymptomatic or experience mild symptoms.Fibrosis and Cirrhosis
Continued inflammation leads to scarring (fibrosis), which can progress to cirrhosis. Liver function declines, and complications such as ascites, variceal bleeding, and hepatic encephalopathy may occur.Hepatocellular Carcinoma (HCC)
In advanced cases, chronic viral hepatitis increases the risk of liver cancer, especially in cirrhotic patients.
Our Treatment Capabilities
CLRD has conducted extensive research on HBV and HCV, including genotyping, immune response studies, and epidemiological surveys. Our treatment protocols are tailored to each patient’s viral type, disease stage, and overall health. Key capabilities include:
Advanced Viral Diagnostics
We use molecular techniques to identify the specific genotype and viral load, which helps in selecting the most effective treatment.Personalized Antiviral Therapy
CLRD offers targeted antiviral medications that suppress viral replication and reduce liver inflammation. For HCV, we use direct-acting antivirals (DAAs) with high cure rates. For HBV, long-term therapy helps control the virus and prevent progression.Stem Cell and Regenerative Therapies
In patients with advanced liver damage, CLRD has successfully used hepatic progenitor cell transplantation to support liver regeneration. These therapies help restore liver function and reduce the need for transplantation.Monitoring and Prevention of Complications
Patients are closely monitored for signs of cirrhosis and liver cancer. Regular imaging and blood tests help detect complications early and guide timely interventions.Counseling and Lifestyle Support
We provide education on preventing transmission, managing diet, and avoiding liver stressors such as alcohol and certain medications.
CLRD’s comprehensive care model has helped thousands of patients achieve viral suppression, reverse liver damage, and improve their quality of life. Our commitment to innovation and patient-centered care ensures the best possible outcomes for those living with chronic viral hepatitis.
Fulminant Hepatic Failure
Fulminant Hepatic Failure (FHF), also known as acute liver failure, is a rare but life-threatening condition where the liver suddenly loses its ability to function, often within days or weeks. Unlike chronic liver diseases that develop over time, FHF strikes rapidly and requires immediate medical attention. At CLRD, we specialize in emergency liver care and have successfully treated critical cases using advanced cellular therapies and supportive interventions.
Symptoms
The symptoms of FHF can escalate quickly and may include:
- Sudden onset of jaundice: Rapid yellowing of the skin and eyes.
- Coagulopathy: Increased tendency to bleed due to impaired clotting factor production.
- Encephalopathy: Confusion, altered consciousness, or coma due to toxin buildup in the brain.
- Nausea and vomiting
- Fatigue and weakness
- Swelling in the abdomen: Due to fluid accumulation (ascites).
These symptoms often appear within a short time frame and can progress to multi-organ failure if not treated promptly.

Stage-wise Progression
Hyperacute Stage (within 7 days)
Symptoms develop very rapidly, often following a viral infection or drug toxicity. Patients may experience severe jaundice and mental confusion.Acute Stage (8–28 days)
Liver function deteriorates further. Blood clotting issues and encephalopathy become more pronounced. Hospitalization is critical.Subacute Stage (4–12 weeks)
The liver shows signs of prolonged damage. Patients may develop complications such as kidney failure, infections, and cerebral edema.
Without timely intervention, FHF can lead to death or necessitate emergency liver transplantation.
Our Treatment Capabilities
CLRD has been a pioneer in managing Fulminant Hepatic Failure using innovative and life-saving therapies. Our approach includes:
Rapid Diagnosis and Monitoring
We use advanced imaging, liver function panels, and neurological assessments to diagnose FHF and monitor its progression in real-time.Intensive Supportive Care
Patients are admitted to specialized liver care units where they receive round-the-clock monitoring, fluid management, and nutritional support.Cellular Therapy Using Fetal Hepatocytes
CLRD has successfully implemented human fetal hepatocyte transplantation in patients with FHF. These cells temporarily take over liver functions, allowing the native liver to recover or bridging the patient to transplantation. This therapy has significantly improved survival rates and reduced complications.Neuroprotective and Anti-inflammatory Protocols
To manage hepatic encephalopathy, CLRD uses targeted therapies that reduce brain swelling and improve cognitive outcomes.Bridging to Transplantation
In cases where liver recovery is not possible, CLRD prepares patients for liver transplantation, ensuring they are stabilized and optimized for surgery.
Our multidisciplinary team, including hepatologists, transplant surgeons, and regenerative medicine experts, works seamlessly to deliver urgent, personalized care. CLRD’s success in treating FHF has saved lives and set new standards in emergency liver medicine.
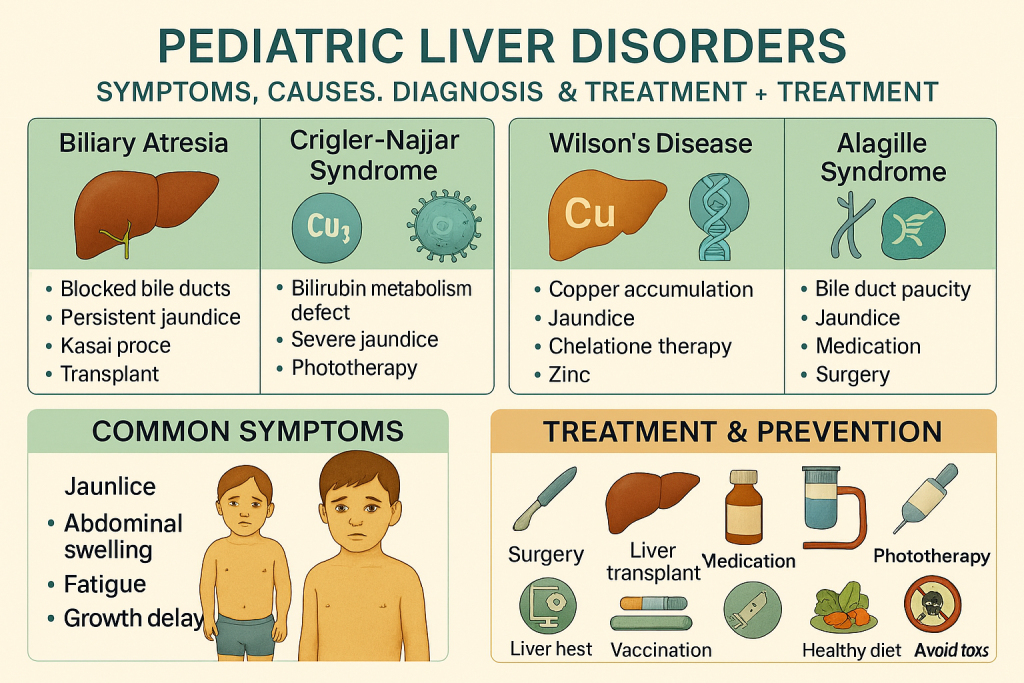
Biliary Atresia and Crigler-Najjar Syndrome
Biliary Atresia and Crigler-Najjar Syndrome are rare but serious liver disorders that primarily affect infants and young children. These conditions interfere with the liver’s ability to process and eliminate bilirubin—a waste product formed during the breakdown of red blood cells. If left untreated, they can lead to severe liver damage and life-threatening complications.
At CLRD, we specialize in pediatric liver care and have successfully treated these conditions using advanced cellular therapies and supportive interventions. Our goal is to restore liver function, reduce bilirubin levels, and improve long-term outcomes for affected children.
Symptoms
Biliary Atresia
- Persistent jaundice beyond two weeks of age
- Pale or clay-colored stools
- Dark urine
- Enlarged liver and spleen
- Slow weight gain and growth delays
Crigler-Najjar Syndrome
- Severe jaundice from birth
- High levels of unconjugated bilirubin in blood
- Risk of kernicterus (bilirubin-induced brain damage)
- No bile duct obstruction (unlike biliary atresia)
Both conditions require early diagnosis and intervention to prevent irreversible liver damage and neurological complications.
Stage-wise Progression
Biliary Atresia
- Early Infancy: Symptoms appear within the first few weeks of life. Liver inflammation begins.
- Progressive Cholestasis: Bile ducts become blocked or absent, leading to bile buildup and liver scarring.
- Cirrhosis and Liver Failure: Without treatment, liver function deteriorates rapidly, often requiring transplantation.
Crigler-Najjar Syndrome
- Type I (Severe): Complete absence of the enzyme needed to process bilirubin. Requires lifelong management and often liver transplantation.
- Type II (Milder): Partial enzyme deficiency. Can be managed with medications but still poses risks if untreated.
Our Treatment Capabilities
CLRD has successfully treated pediatric liver conditions using hepatic progenitor cell transplantation, offering a breakthrough alternative to traditional therapies. Our capabilities include:
Early Diagnosis and Genetic Screening
We use advanced diagnostic tools to identify these conditions early, including enzyme assays, liver imaging, and genetic testing.Cellular Therapy for Liver Support
CLRD has pioneered the use of hepatic progenitor cells to manage hyperbilirubinemia in both biliary atresia and Crigler-Najjar Syndrome. These cells help restore liver function and reduce bilirubin levels, offering a bridge to recovery or delaying the need for transplantation.Minimally Invasive Transplantation Techniques
Our team has developed safe and effective methods for delivering stem cells via the hepatic artery or peritoneal cavity, minimizing risk and maximizing therapeutic benefit.Comprehensive Pediatric Liver Care
Children receive holistic care including nutritional support, phototherapy (for Crigler-Najjar), and monitoring for neurological and developmental milestones.Long-Term Follow-Up and Family Counseling
We provide ongoing support to families, helping them understand the condition, manage treatment, and prepare for future needs such as transplantation if required.
CLRD’s innovative approach has transformed the management of these rare liver disorders, giving children a chance at a healthier life and reducing the burden on families. Our success stories reflect our commitment to excellence in pediatric liver care.
At the Center for Liver Research and Diagnostics (CLRD), our mission is to provide transformative care for patients suffering from chronic liver diseases—whether genetic, viral, toxic, or lifestyle-induced. Across conditions such as Alpha-1-Antitrypsin Deficiency, Alcoholic Liver Disease, Toxin-Induced Liver Injury, Viral Hepatitis, Fulminant Hepatic Failure, and rare pediatric disorders like Biliary Atresia and Crigler-Najjar Syndrome, CLRD has consistently delivered innovative, patient-centric solutions.
Our strength lies in a multidisciplinary approach that integrates:
- Advanced diagnostics for early and accurate detection
- Personalized pharmacotherapy tailored to each patient’s condition and progression
- Regenerative medicine, including stem cell and hepatic progenitor cell therapies, to restore liver function
- Lifestyle and nutritional counseling to support long-term recovery
- Emergency interventions for acute liver failure and pediatric liver disorders
Backed by decades of research and clinical success, CLRD has not only improved survival rates but also enhanced the quality of life for thousands of patients. Our commitment to innovation, compassion, and excellence ensures that every individual receives care that is both scientifically advanced and deeply human.
Whether facing a newly diagnosed liver condition or managing a complex, long-standing disease, patients at CLRD find hope, healing, and a path forward.
