Amoebic Liver Abscess
Amoebic Liver Abscess (ALA) is one of the most common and serious forms of extraintestinal amoebiasis, and at the Centre for Liver Research and Diagnostics (CLRD), we have been at the forefront of its diagnosis, treatment, and research for over four decades. Our institution has played a pivotal role in shaping the understanding of this condition, not only in India but globally, through extensive clinical studies and innovative therapeutic approaches.
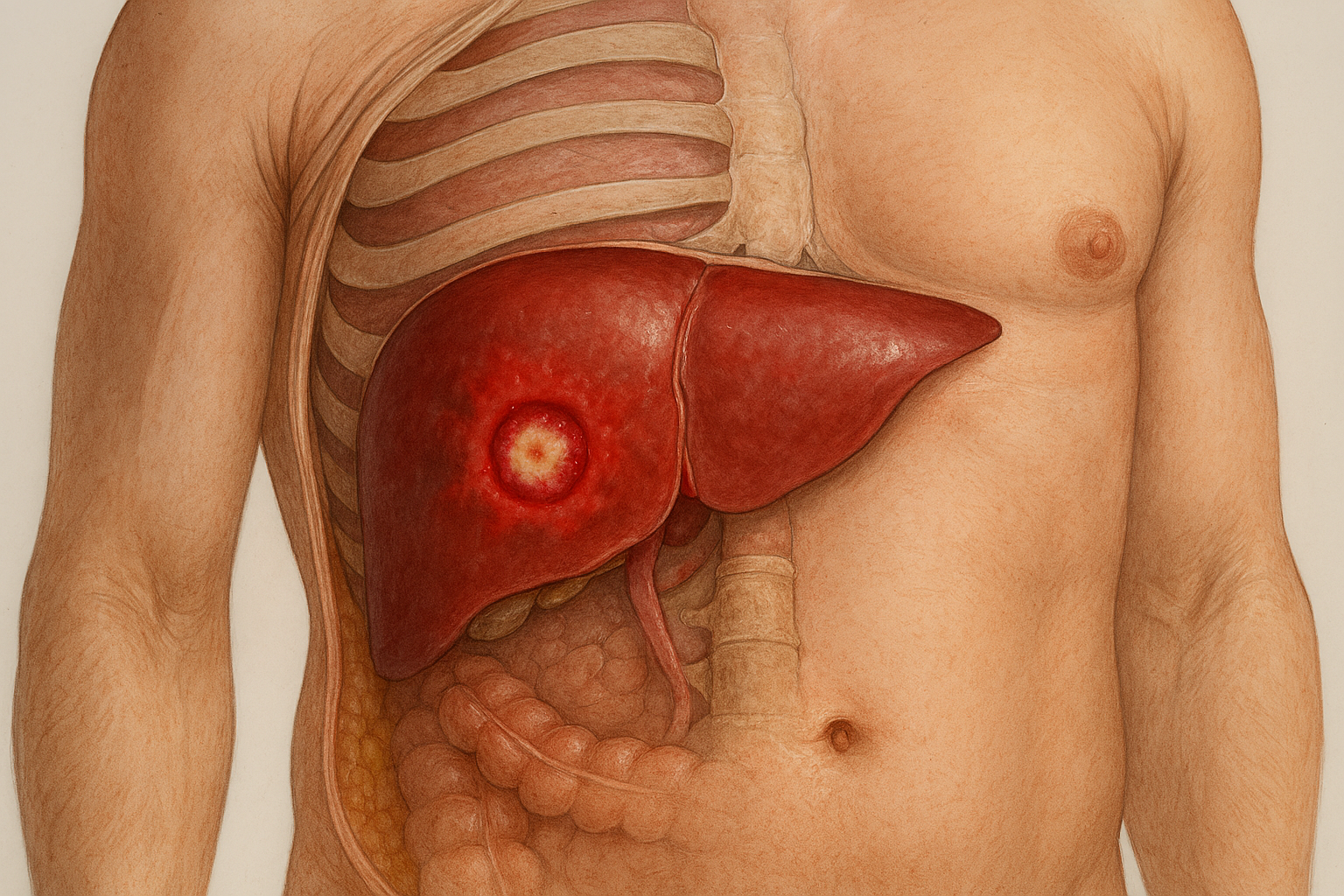
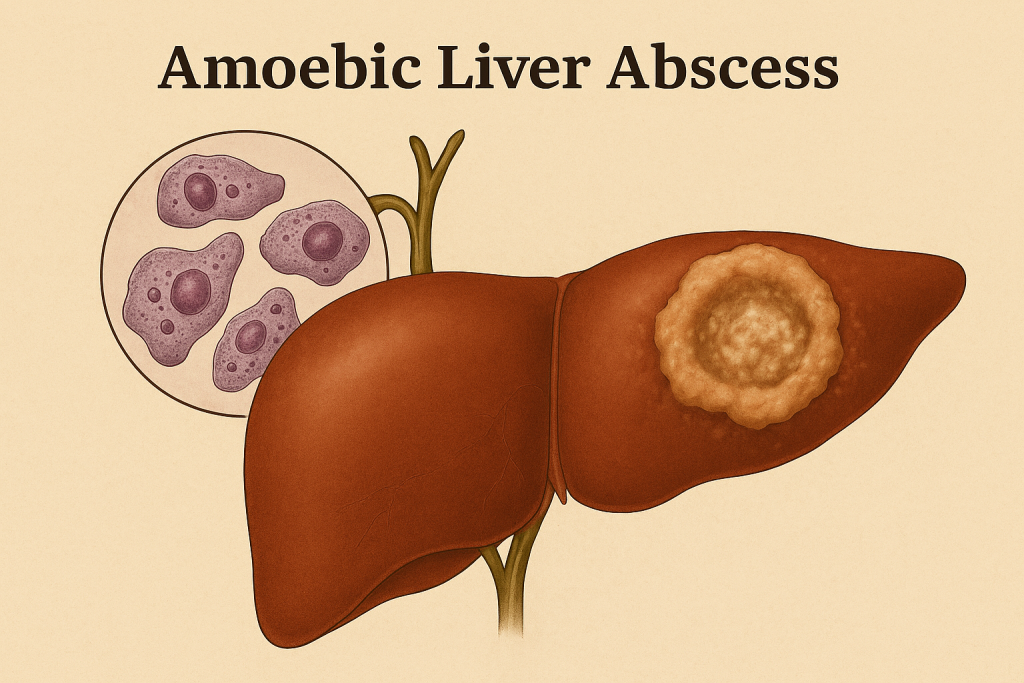
ALA is caused by the parasite Entamoeba histolytica, which typically infects the intestine but can migrate to the liver, forming pus-filled cavities known as abscesses. At CLRD, we have developed and refined diagnostic techniques that allow for early and accurate identification of these abscesses. Our pioneering work in serial liver scanning has enabled clinicians to monitor the resolution of abscesses over time, ensuring that treatment is both effective and responsive to the patient’s progress. We have also utilized advanced ultrasound imaging to differentiate ALA from other hepatic conditions such as hydatid cysts, which can present with similar symptoms but require entirely different management.
Beyond imaging, CLRD has conducted extensive immunological research to understand the host’s response to amoebic infection. Through ELISA-based serodiagnosis and lymphokine assays, we have been able to identify immune markers that guide treatment decisions and predict outcomes. Our experimental models in rats and mice have further deepened our understanding of hepatic amoebiasis, including the mechanisms of immune transfer and the role of host genetics in susceptibility.
Thanks to these research-backed insights, CLRD has established highly effective treatment protocols that combine targeted antimicrobial therapy with immunomodulatory support. These protocols have consistently resulted in high cure rates, even in complex or recurrent cases. As a result, CLRD has become a trusted referral center for ALA cases across India, known for its diagnostic precision, compassionate care, and clinical success.
Symptoms
Patients with Amoebic Liver Abscess typically present with a range of symptoms that may vary depending on the stage and severity of the infection. Common symptoms include:
- Persistent fever, often with chills
- Pain in the upper right abdomen
- Generalized fatigue and malaise
- Jaundice in advanced cases
- Occasionally, cough or chest pain if the abscess is near the diaphragm
Early recognition of these symptoms is crucial for timely intervention and to prevent complications such as rupture of the abscess or spread to other organs.
Precautions
Preventing ALA involves a combination of hygiene practices and public health awareness. Patients and caregivers should be mindful of the following precautions:
- Ensure safe drinking water, preferably boiled or filtered
- Maintain proper sanitation and hand hygiene, especially after using the toilet and before meals
- Avoid consumption of raw or undercooked food in endemic areas
- Seek medical attention promptly if gastrointestinal symptoms persist, especially in regions known for amoebiasis
- Follow prescribed medication regimens strictly and attend follow-up imaging sessions to confirm resolution
For individuals who have recovered from ALA, regular liver health check-ups are recommended to monitor for any residual effects or recurrence.
Stage-wise Progression
The progression of Amoebic Liver Abscess typically follows a predictable pattern:
- Initial Stage (Invasion): The parasite invades the intestinal wall and migrates to the liver via the portal vein. Symptoms may be mild or absent at this stage.
- Formation Stage (Abscess Development): The liver begins to form one or more abscesses. Patients experience fever, pain, and systemic symptoms. Imaging studies reveal characteristic lesions.
- Complication Stage (Advanced Disease): If untreated, the abscess may enlarge or rupture, leading to peritonitis, pleural effusion, or secondary infections. Jaundice and systemic toxicity may develop.
- Resolution Stage (Post-Treatment Recovery): With appropriate therapy, the abscess resolves. Follow-up imaging confirms healing, and symptoms gradually subside. Immunological markers normalize.
At CLRD, we manage each stage with precision, ensuring that patients receive timely interventions tailored to their clinical status. Our multidisciplinary team of hepatologists, infectious disease specialists, and radiologists work together to deliver holistic care that addresses both the infection and its systemic impact.
