Ulcerative Colitis & Crohn’s Disease
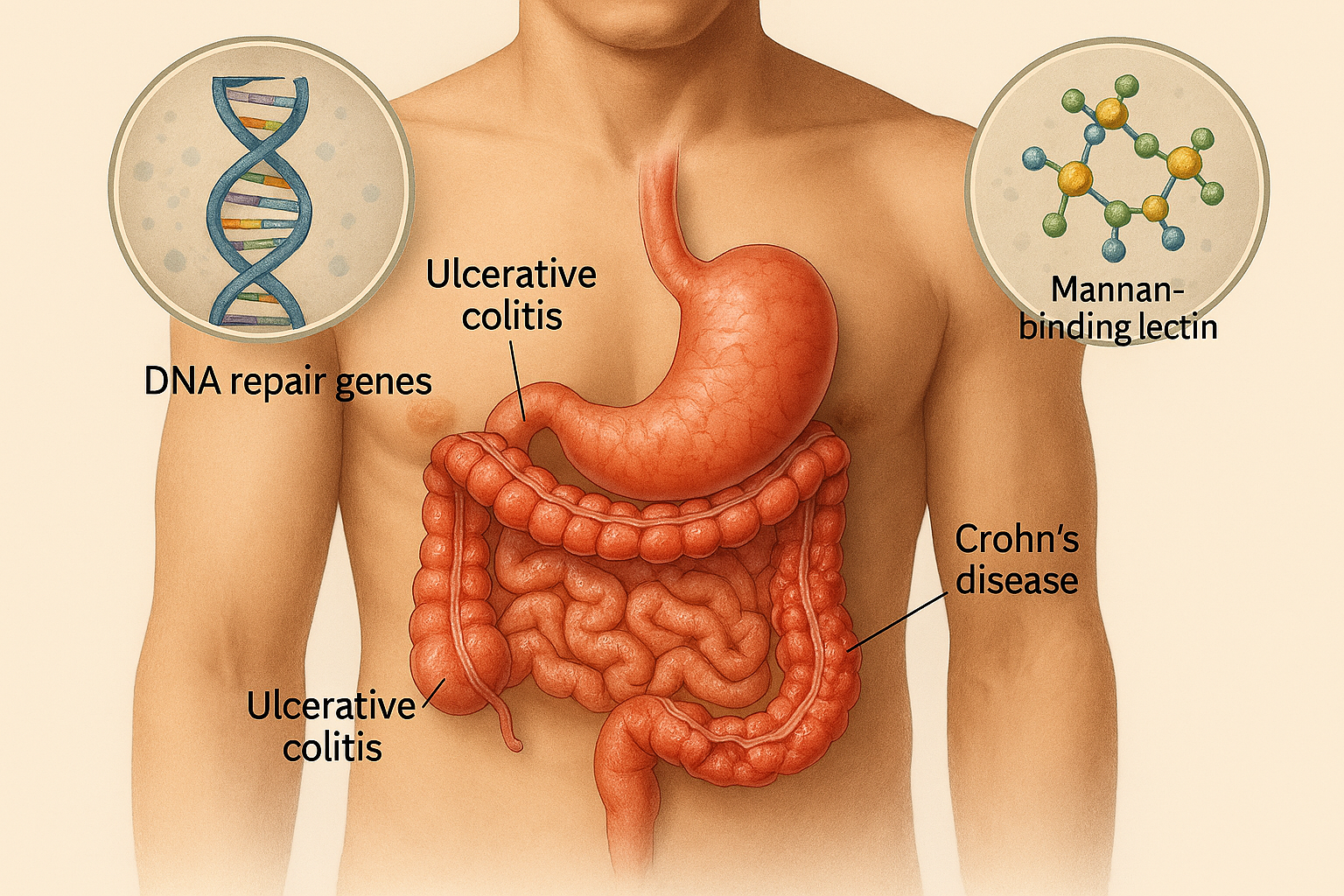
Ulcerative Colitis (UC) and Crohn’s Disease (CD) are chronic, relapsing inflammatory bowel diseases (IBD) that primarily affect the gastrointestinal tract.
- Ulcerative Colitis involves continuous inflammation of the colonic mucosa, starting from the rectum and extending proximally.
- Crohn’s Disease, in contrast, is characterized by transmural inflammation that can affect any part of the GI tract, most commonly the terminal ileum and colon, with skip lesions and complications such as strictures and fistulas.
Both conditions result from a complex interplay of genetic susceptibility, immune dysregulation, environmental triggers, and gut microbiota alterations. Patients often present with abdominal pain, diarrhea (sometimes bloody), weight loss, and systemic symptoms like fatigue.
Pathophysiology
IBD pathogenesis involves:
- Immune Dysregulation: Overactive immune response against intestinal microbiota leads to chronic inflammation.
- Genetic Factors: Variants in genes regulating DNA repair and innate immunity predispose individuals to disease.
- Barrier Dysfunction: Impaired epithelial integrity allows luminal antigens to trigger immune activation.
CLRD’s Research Contributions
The Centre for Liver and Digestive Research (CLRD) has significantly advanced the understanding of IBD through immunogenetic and molecular studies, focusing on South Indian populations to provide globally relevant insights.
Genetic Insights
- DNA Repair Genes (XRCC-1, APE-1):
CLRD identified functional polymorphisms in these genes, linking defective DNA repair mechanisms to increased mucosal vulnerability and chronic inflammation. - Mannan Binding Lectin (MBL) Variants:
Our studies demonstrated that MBL gene polymorphisms alter innate immune responses, influencing susceptibility and severity of UC and CD.
Epidemiological Studies
- CLRD conducted large-scale prevalence studies in South India, revealing unique demographic and genetic patterns of IBD.
- These findings contributed to global IBD registries, improving understanding of disease heterogeneity across populations.
Molecular and Immunological Profiling
- Analysis of cytokine signatures and immune cell phenotypes provided insights into disease activity and therapeutic targets.
- Identification of biomarkers for early diagnosis and prognosis, aiding personalized treatment strategies.
Diagnostic Approaches
CLRD integrates conventional and advanced diagnostic modalities:
- Endoscopy: Colonoscopy with biopsy remains the gold standard for diagnosis and disease staging.
- Histopathology: Confirms chronic inflammatory changes and differentiates UC from CD.
- Genetic Testing: Screening for XRCC-1, APE-1, and MBL variants for risk stratification.
- Serological Markers: pANCA and ASCA antibodies for differential diagnosis.
- Imaging: MRI enterography and CT scans for assessing complications like strictures and fistulas.
Therapeutic Insights
- CLRD’s research supports biologic therapies targeting TNF-α and integrins for refractory cases.
- Exploration of nutritional interventions and microbiome modulation as adjunct strategies.
- Contribution to regional treatment guidelines for cost-effective and evidence-based care.
Impact and Future Directions
- CLRD’s work has shaped global understanding of IBD genetics and immunology, influencing therapeutic innovations.
- Future research aims at precision medicine, leveraging genomic and microbiome data for individualized care.
