Gastric Carcinoma
Gastric carcinoma, commonly referred to as stomach cancer, is one of the leading causes of cancer-related mortality worldwide. It originates from the epithelial lining of the stomach and is often associated with chronic gastritis, intestinal metaplasia, and infection by Helicobacter pylori. The disease typically progresses silently, with early stages being asymptomatic or presenting vague symptoms such as dyspepsia, weight loss, and fatigue. Advanced stages may manifest with epigastric pain, vomiting, hematemesis, and anemia.
Globally, gastric carcinoma remains a major health burden, and in India, its incidence is rising due to dietary habits, genetic predisposition, and high prevalence of H. pylori infection.
Pathophysiology
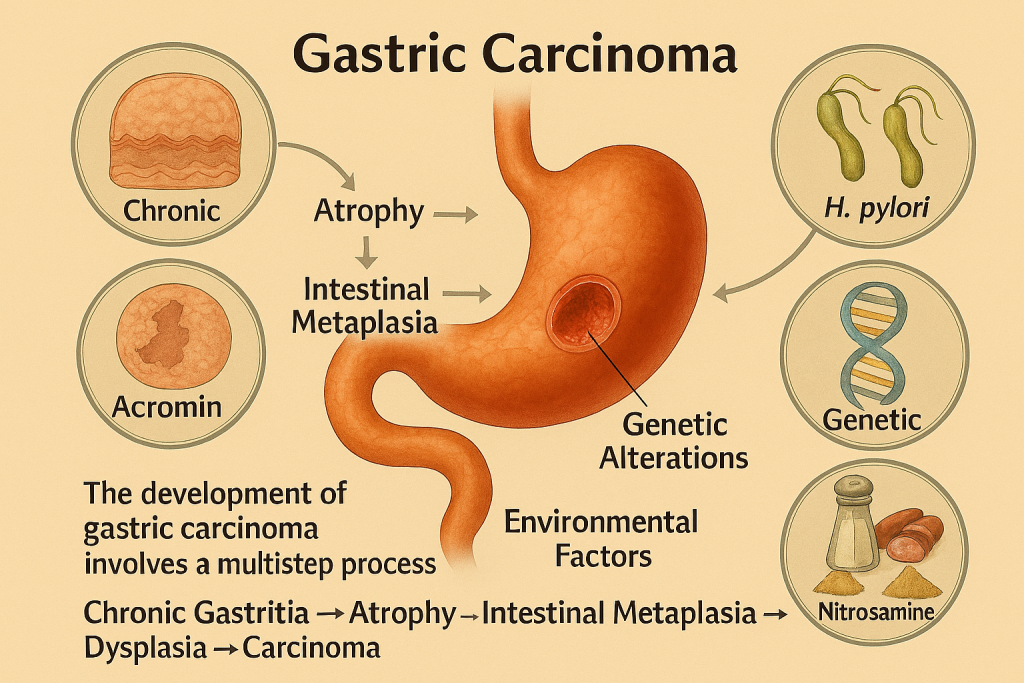
The development of gastric carcinoma involves a multistep process:
- Chronic Gastritis → Atrophy → Intestinal Metaplasia → Dysplasia → Carcinoma
- H. pylori Infection: Plays a central role by inducing chronic inflammation and producing virulence factors such as CagA and VacA, which disrupt cellular signaling and promote carcinogenesis.
- Genetic Alterations: Mutations in tumor suppressor genes and DNA repair pathways accelerate malignant transformation.
- Environmental Factors: High salt intake, smoked foods, and nitrosamines increase risk.
CLRD’s Research Contributions
The Centre for Liver and Digestive Research (CLRD) has made pioneering contributions to understanding gastric carcinoma through molecular genetics, immunology, and epidemiology.
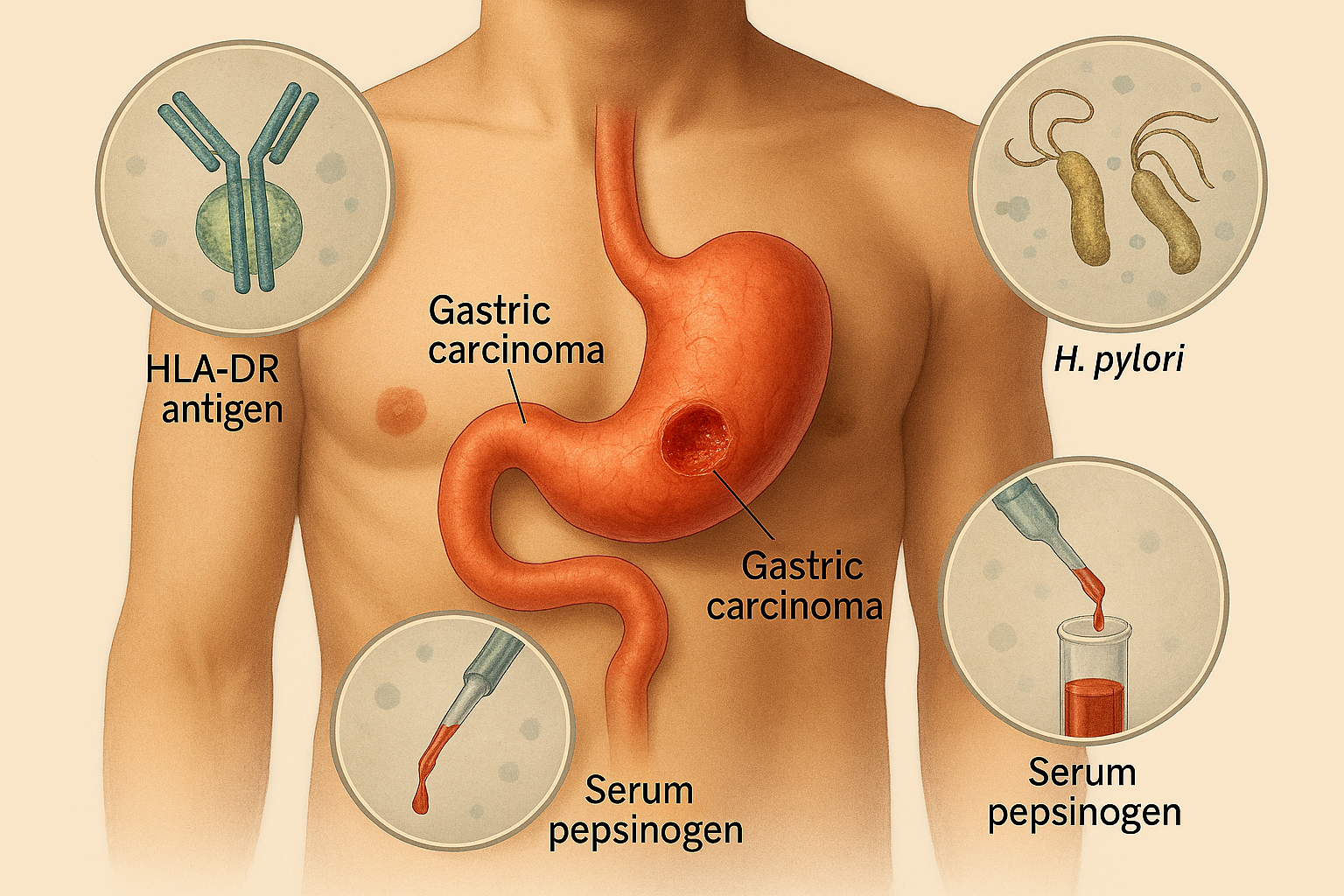
HLA-DR Antigen Associations
- CLRD identified a strong correlation between HLA-DR antigen expression and susceptibility to gastric carcinoma.
- These findings provided insights into immune-mediated mechanisms in gastric cancer pathogenesis.
Serum Pepsinogen Levels
- Our studies demonstrated that low serum pepsinogen I and high pepsinogen II levels serve as biomarkers for gastric mucosal atrophy and cancer risk.
- This research laid the foundation for non-invasive screening programs.
Molecular Genotyping of H. pylori
- CLRD performed extensive genotyping of H. pylori virulence genes (cagA, vacA) in Indian populations.
- These studies revealed unique bio-geographic signatures and their association with gastric cancer prognosis.
Diagnostic Approaches
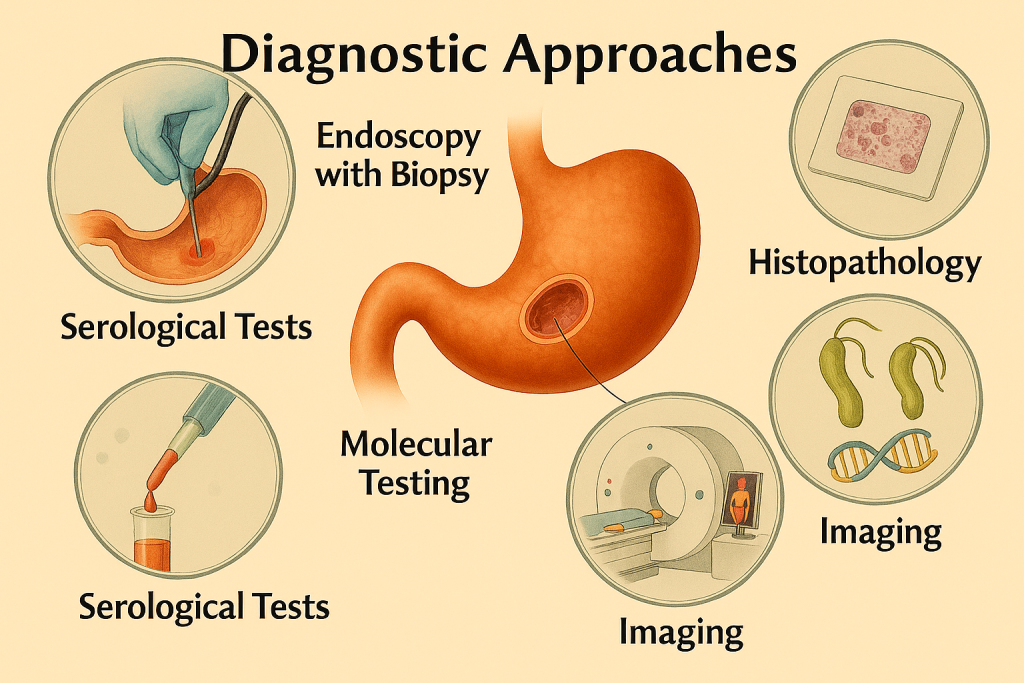
CLRD integrates conventional and advanced diagnostic modalities:
- Endoscopy with Biopsy: Gold standard for diagnosis and staging.
- Histopathology: Confirms adenocarcinoma and subtypes (intestinal vs. diffuse).
- Serological Tests: Pepsinogen assays for risk stratification.
- Molecular Testing: Detection of H. pylori virulence genes and genetic markers.
- Imaging: CT and PET scans for staging and metastasis evaluation.
Therapeutic Insights
- CLRD’s research supports early detection strategies to improve survival.
- Contribution to chemotherapy protocols and exploration of targeted therapies based on molecular profiling.
- Advocacy for H. pylori eradication programs as a preventive measure.
Impact and Future Directions
- CLRD’s work has influenced national cancer screening guidelines and improved understanding of gastric cancer biology.
- Future research focuses on genomic risk prediction, liquid biopsy biomarkers, and personalized therapy.
