Fulminant Hepatic Failure (FHF)
At the Centre for Liver Research and Diagnostics (CLRD), we are committed to transforming the landscape of liver disease treatment through pioneering research and compassionate care. Among our core specializations, the management of Fulminant Hepatic Failure (FHF) stands as a testament to our relentless pursuit of innovation and excellence. FHF, a rapidly progressing and life-threatening condition, demands swift and sophisticated intervention. At CLRD, we have not only met this challenge but have redefined its treatment paradigm through groundbreaking therapies such as human fetal hepatocyte transplantation, bioartificial liver systems, and xenotransplantation models. Our patient-centric approach ensures that every individual receives personalized, evidence-based care, supported by decades of internationally recognized research and clinical success.

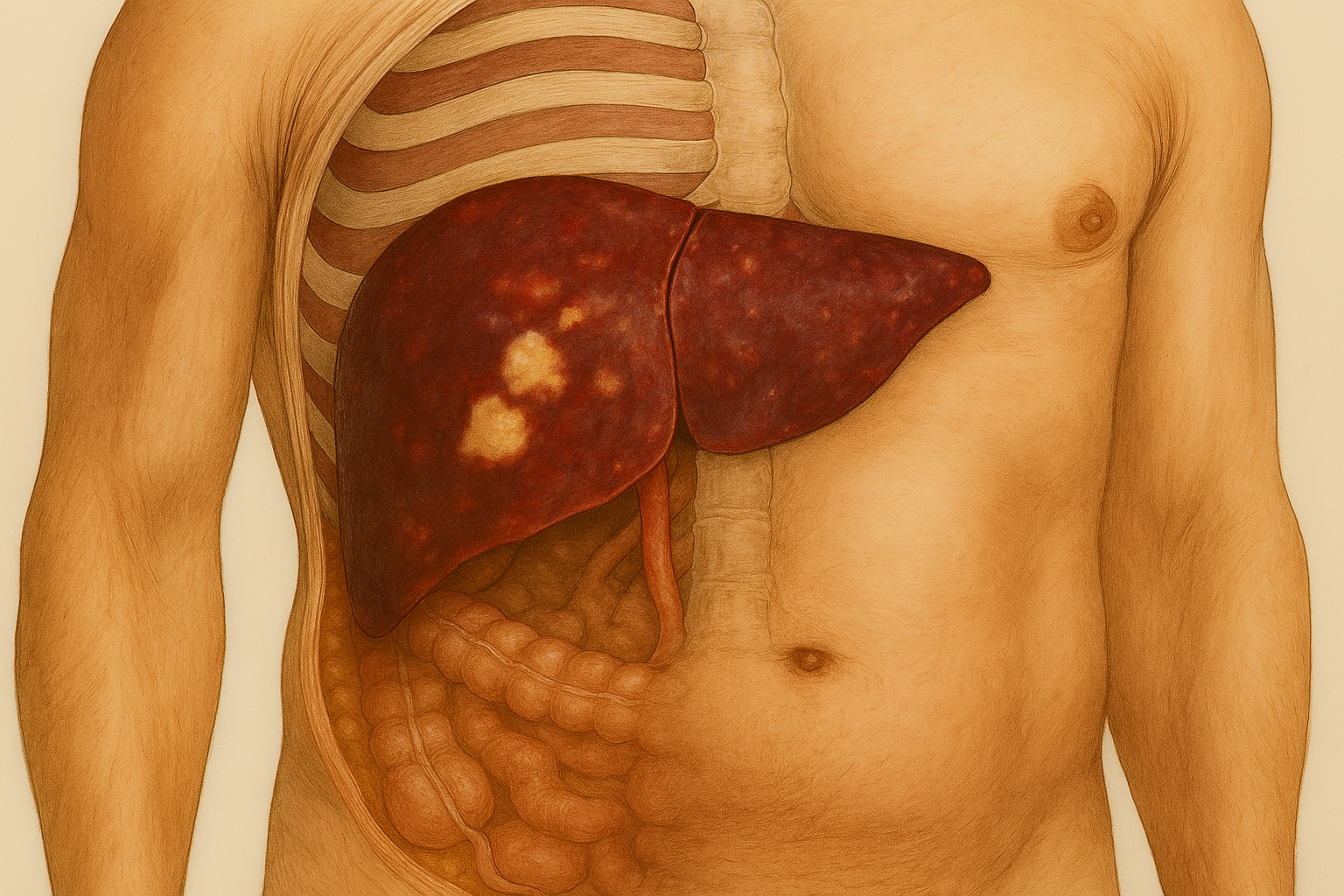
Fulminant Hepatic Failure (FHF) is a rare but devastating clinical syndrome characterized by the rapid deterioration of liver function in individuals without pre-existing liver disease. At CLRD, we have developed a comprehensive and innovative treatment protocol that has saved countless lives. Our center was the first in India to perform human fetal hepatocyte transplantation in FHF patients, a pioneering achievement that has since become a cornerstone of our therapeutic approach. This procedure involves the transplantation of metabolically active fetal liver cells, which temporarily assume the liver’s vital functions, providing a crucial bridge to either spontaneous hepatic regeneration or liver transplantation.
Our capabilities extend beyond transplantation. CLRD has been at the forefront of developing bioartificial liver support systems using microencapsulated hepatocytes, which simulate the liver’s detoxification and metabolic roles. These systems are particularly effective in stabilizing patients during the critical window of liver failure, reducing the risk of multi-organ dysfunction and buying time for recovery or definitive surgical intervention.
In addition, CLRD has pioneered the use of UV-B irradiated hepatocytes and xenotransplantation models, which have demonstrated enhanced immunological compatibility and improved survival of transplanted cells. These techniques, validated through rigorous preclinical and clinical studies, have significantly reduced immune rejection and improved therapeutic outcomes.
Our treatment protocols are deeply rooted in decades of research, with landmark studies published in prestigious journals such as Transplantation (1994), Liver (1995), and International Hepatology Communication (1995). These publications document our success in xenogenic transplantation, UV-B hepatocyte irradiation, and bioartificial liver development, establishing CLRD as a global leader in regenerative hepatology.
Furthermore, CLRD’s multidisciplinary team of hepatologists, transplant surgeons, regenerative medicine experts, and critical care specialists work in unison to deliver holistic care. From early diagnosis and intensive care to advanced cellular therapies and post-recovery rehabilitation, our infrastructure is equipped to manage the full spectrum of FHF with precision and empathy.
Symptoms
Patients with FHF often present with a rapid onset of symptoms, which may include:
- Sudden onset of jaundice (yellowing of the skin and eyes)
- Confusion, disorientation, or altered mental status (hepatic encephalopathy)
- Nausea, vomiting, and loss of appetite
- Severe fatigue and weakness
- Abdominal pain and swelling due to fluid accumulation (ascites)
- Bleeding or bruising easily due to impaired blood clotting
- Seizures or progression to coma in advanced stages
Prompt recognition and immediate medical attention are critical, as the condition can deteriorate rapidly.

Stage-wise Progression
Hyperacute Phase (Within 7 Days): Characterized by the sudden appearance of jaundice and coagulopathy, often accompanied by mild confusion or drowsiness. Liver enzymes are significantly elevated, and INR levels rise rapidly.
Acute Phase (8–28 Days): The patient may develop worsening hepatic encephalopathy, increasing coagulopathy, and signs of systemic inflammation. Renal dysfunction and metabolic disturbances may emerge.
Subacute Phase (Beyond 28 Days): This stage is marked by deepening coma, severe coagulopathy, cerebral edema, and multi-organ failure. Without timely intervention, the prognosis becomes extremely poor.
At CLRD, our early diagnostic algorithms and rapid deployment of advanced therapies such as hepatocyte transplantation and bioartificial liver support have significantly improved survival rates, even in patients presenting in the late stages of FHF.
Our Treatment Capabilities
CLRD’s capabilities in managing Fulminant Hepatic Failure are unmatched in the region and recognized globally. Our center is equipped with:
- Dedicated Hepatocyte Transplantation Units with sterile, GMP-compliant facilities for isolating and preserving human fetal hepatocytes.
- Bioartificial Liver Support Systems developed in-house, incorporating encapsulated hepatocytes for extracorporeal detoxification.
- Advanced Xenotransplantation Models using UV-B irradiated hepatocytes to enhance graft survival and reduce immune rejection.
- Critical Care Infrastructure tailored for FHF patients, including intensive monitoring, neurocritical care, and renal replacement therapies.
- Multidisciplinary Expertise in hepatology, regenerative medicine, immunology, and transplant surgery, ensuring comprehensive and personalized care.
- Research-Driven Protocols backed by over three decades of peer-reviewed publications, clinical trials, and translational research.
Our integrated approach ensures that patients with FHF receive not only life-saving interventions but also long-term support for recovery and quality of life restoration.
Use of Bioartificial Liver System

The Bioartificial Liver (BAL) system is a life-saving therapeutic device developed at CLRD to support patients suffering from Fulminant Hepatic Failure (FHF). This system is designed to temporarily replicate the detoxification, synthetic, and regulatory functions of the human liver, providing critical support until the patient’s liver regenerates or a liver transplant becomes available.
At CLRD, the BAL system is built using microencapsulated hepatocytes, which are liver cells enclosed in semi-permeable biocompatible capsules. These capsules allow the exchange of nutrients, oxygen, and waste products while protecting the hepatocytes from immune attack. The encapsulated cells are housed in a bioreactor that is connected to the patient’s blood circulation through an extracorporeal circuit, similar to dialysis.
The primary function of the BAL system is to detoxify the blood, removing ammonia, bilirubin, and other harmful metabolites that accumulate during liver failure. It also contributes to protein synthesis, urea cycle activity, and metabolic regulation, which are essential for maintaining homeostasis in critically ill patients.
CLRD’s research, including the 2002 study by Aleem et al. (Indian Journal of Gastroenterology, 21(2): 55–58), demonstrated the efficacy of goat hepatocyte-based BAL modules in vitro, which laid the foundation for further development using human fetal hepatocytes. These systems have been refined over the years to improve cell viability, metabolic activity, and biocompatibility, making them suitable for clinical application.
The BAL system is particularly valuable in:
- Bridging patients to liver transplantation by stabilizing their condition.
- Supporting spontaneous liver regeneration in cases where recovery is possible.
- Reducing the risk of multi-organ failure by maintaining metabolic balance.
CLRD’s BAL technology is unique in its integration of regenerative medicine and bioengineering, offering a non-invasive, cell-based alternative to conventional liver support. It is especially beneficial in resource-limited settings where immediate access to liver transplantation is not feasible.
